by Alex | Jun 8, 2017 | family health insurance, group health insurance, Health Care Reform, Health Exchanges, Individual Exchanges, NY News
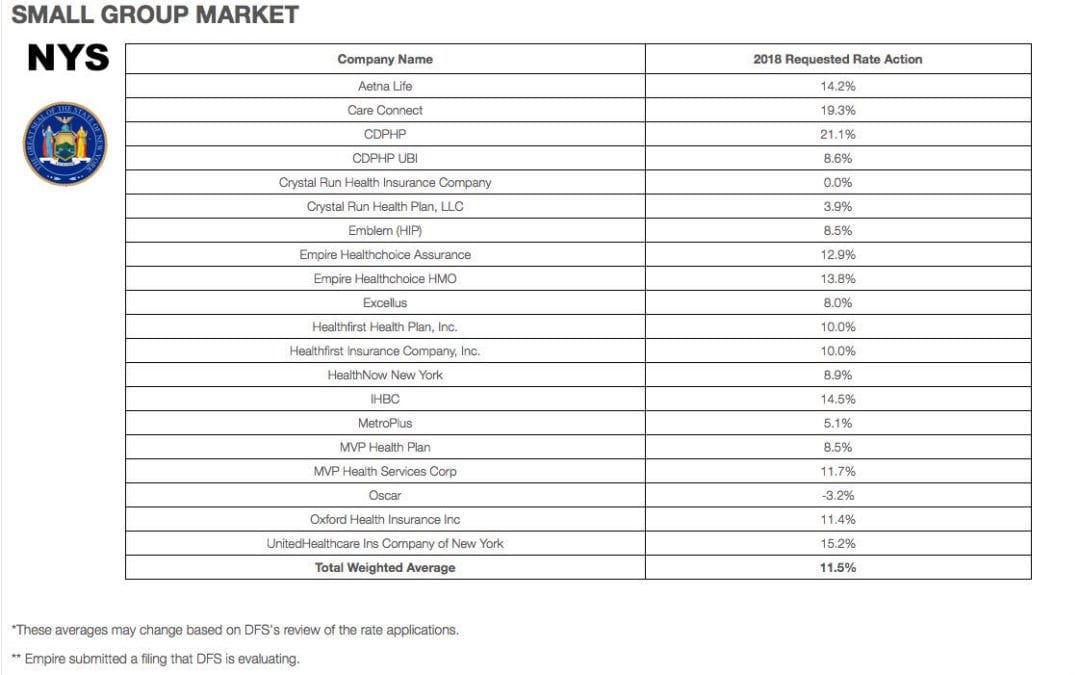
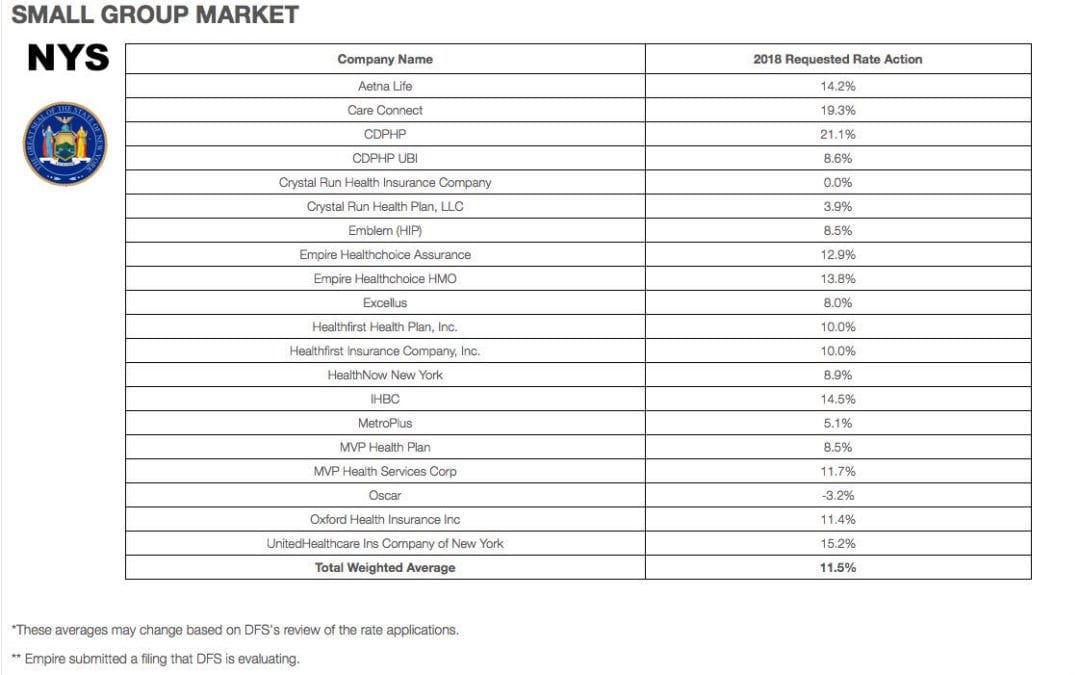
NYS 2018 Health Insurance Rate Filing
Yesterday, NYS 2018 Health Insurance Rate Filing were released. The total weighted average increases were 11.5% small groups and 16.6% individual market. This early filing request deadline request requirement is not an Obamacare requirement. As per NY State Law carriers are required to send out notices of rate increase filings to groups and subscribers.
These are simply requests and the state’s Department of Financial Services has authority to modify the final rates. But they are the first indication of what New Yorkers can expect when shopping for health insurance on the individual marketplace at the end of this year. The news comes as insurance companies across the country brace consumers for another year of large rate hikes, owing in part to the composition of the individual market, and in part to the uncertainty over the future of the law under the Trump administration.
Background:
By comparison last year NYS 2017 Rate Request early filings were higher at 12.3% small group and 19.3% for individuals. The final filing rates were lower NYS 2017 Final Rates were 8.3% small group and 16.6% for individuals. The NYS 2016 Rates final rates were 9.8% small group and 7.1% for individuals. Using these past figures one projects a 2018 Final Rates of 7% small groups and 14% individuals.
With only 3 months of mature claims in 2017 to work of off Insurance Actuaries have little experience to predict accurate projections. Simply put the less credible information presented to actuarial the higher the uncertainly and higher than expected rate increase. The national rate trend, however, has been much higher than in past years due to higher health care costs and the loss of Federal reinsurance fund known as risk reinsurance corridor.
Individuals:

Individual rates are expected to be higher than small group. The national rate trend, however, has been much higher than in past years due to higher health care costs Like other states throughout the nation, the 2018 rate of increase for individuals in New York is higher than in past years partly due to the termination of the federal reinsurance program. The lost of the program’s aka federal risk reinsurance corridor funds accounts for 5.5 percent of the rate increase.
This is one of the reasons why the individual market is significantly more costly to operate than small group as per recent Aetna and United Healthcare pull out of most State Individual Exchanges. Another local example was last year’s Oscar Health Insurance which had lost $105 million and is asking for up to 30% rate increase. The 3 year old company said the increase was necessary because medical costs have risen, government programs that helped cover costs are ending, and its members needed more care than expected. For 2018, with successful pivotal changes Oscar is asking below average 11% individual increase and a decrease of 3.2% small group next year.
Small Groups:
While small group rates are better risk and naturally lower rates. There is some rate shock with notably Careconnect. CareConnect, the financially struggling health insurance arm of Northwell Health, has asked the Cuomo administration to allow an average 30 percent premium hike on the individual market in 2018. The company, which lost $157 million in 2016, is asking for small group increases that range between 9 and 24 percent.
THE THREE R – RISK CORRIDOR, RISK ADJUSTMENT & REINSURANCE designed to mitigate the adverse selection and risk selection. The problem, according to many insurance companies, is that the formula is flawed, and CareConnect executives have consistently complained that they are at an unfair disadvantage. The Cuomo administration has taken steps to ameliorate some of those problems, giving the DFS the authority to essentially overrule the federal numbers. In its first-quarter financial report, executives made clear that the risk adjustment penalty was a threat to its business.
Instead, the correct approach for a small business in keeping with simplicity is a Private Exchange. This is a true defined contribution empowering employees with choice of leading insurers offering paperless technologies integrating HRIS/Benefits/Payroll. Both employee and employers still gain tax advantage benefits under the business. Also, the benefits, rates and network size are superior under a group plan as THE RISK OUTLINED ABOVE ARE HIGHER FOR INDIVIDUAL MARKETS THAN SMALL GROUP PLANS.
You may view the NYS 2018 Rate Requests DFS press release, which includes a recap of the increases requested and approved by clicking here.
For a custom analysis comparing PEO with YOUR upcoming 2017-2018 renewal please contact our team at 36PEO (855)667-4621. We work in coordination with Navigators to assist with Medicaid, CHIP Child Health Plus, Family Health Plus and Medicare Dual Eligibles. We have Spanish, Russian, and Hebrew speakers available. Quotes can also be viewed on our site.
Summary of 2018 Requested Rate Actions
INDIVIDUAL MARKET
| Company Name | 2018 Requested Rate Action |
|---|
| Affinity | 23.5% |
| Care Connect | 29.7% |
| CDPHP | 15.2% |
| Crystal Run Health Plan, LLC | 8.7% |
| Emblem (HIP) | 24.9% |
| Empire ** | N/A |
| Excellus | 4.4% |
| Fidelis | 8.5% |
| Healthfirst Insurance Company, Inc. | 13.0% |
| Healthfirst PHSP, Inc. | 22.1% |
| HealthNow New York | 47.3% |
| IHBC | 25.9% |
| MetroPlus | 7.9% |
| MVP Health Plan | 13.5% |
| Oscar | 11.1% |
| UnitedHealthcare of New York Inc | 38.5% |
| Total Weighted Average | 16.6% |
SMALL GROUP MARKET
| Company Name | 2018 Requested Rate Action |
|---|
| Aetna Life | 14.2% |
| Care Connect | 19.3% |
| CDPHP | 21.1% |
| CDPHP UBI | 8.6% |
| Crystal Run Health Insurance Company | 0.0% |
| Crystal Run Health Plan, LLC | 3.9% |
| Emblem (HIP) | 8.5% |
| Empire Healthchoice Assurance | 12.9% |
| Empire Healthchoice HMO | 13.8% |
| Excellus | 8.0% |
| Healthfirst Health Plan, Inc. | 10.0% |
| Healthfirst Insurance Company, Inc. | 10.0% |
| HealthNow New York | 8.9% |
| IHBC | 14.5% |
| MetroPlus | 5.1% |
| MVP Health Plan | 8.5% |
| MVP Health Services Corp | 11.7% |
| Oscar | -3.2% |
| Oxford Health Insurance Inc | 11.4% |
| UnitedHealthcare Ins Company of New York | 15.2% |
| Total Weighted Average | 11.5% |
*These averages may change based on DFS’s review of the rate applications.
** Empire submitted a filing that DFS is evaluating.

by Alex | Feb 15, 2017 | Health Care Reform, Obamacare, PPACA, State Exchanges
 Leading article on the direction of TRUMPCARE we’ve read thus far. Former president Barack Obama’s budget director, Peter Orszak thinks Obamacare will be replaced through the waiver process.
Leading article on the direction of TRUMPCARE we’ve read thus far. Former president Barack Obama’s budget director, Peter Orszak thinks Obamacare will be replaced through the waiver process.
Here’s How Trump Will Change Obamacare
By Peter R. Orszag FEB 14, 2017 6:00 AM EST
Promises made by Donald Trump and Republicans in Congress to repeal and replace the Affordable Care Act are proving to be more complicated than they sounded on the campaign trail. With reality now setting in, what’s most likely to happen?
I expect to see Republicans stage a dramatic early vote to repeal, with legislation that includes only very modest steps toward replacement — and leave most of the work for later. Next, the new administration will aggressively issue waivers allowing states to experiment with different approaches, including changes to Medicaid and private insurance rules. At some point, then, the administration will declare that these state experiments have been so successful, Obamacare no longer exists.
In other words, the repeal vote will be just for show; the waivers will do most of the heavy lifting.
I predict something like this will happen because of two core challenges that stand in the way of Republicans’ replacing the ACA through legislation: the need for so-called community rating and the need to have 60 votes in the Senate to pass a comprehensive new health-care law.
First, community rating. It is one of the basic building blocks needed to create a workable private insurance market — whether Democrats or Republicans are doing the building. If your insurance covers a pre-existing condition but at a cost of, say, $100,000, that doesn’t really help. Community rating requires that your premium be the same as that of other people in your area, no matter how unhealthy you are.
With community rating in place, the next step is to recognize how easy it is to game the system: People can just wait until they get sick, then buy insurance at the community rate. To discourage that practice, the system needs to give people some strong incentive to purchase insurance before they get sick. The Affordable Care Act used an individual mandate; most Republican plans instead propose a requirement for continuous coverage. That is, people enjoy access to community-rated premiums in the future only if they have kept themselves insured over some period of time in the past.
Given the costs involved, subsidies are also needed to ensure that low- and moderate-income households can afford the coverage. This overall structure means that younger, healthier people implicitly subsidize older, sicker people.
Such are the inescapable constraints imposed by community rating. Community rating could be discarded, as Mark Pauly of the University of Pennsylvania has argued. Pauly instead proposes that insurance companies be allowed to vary people’s premiums according to their health status, and that general revenue be used to pay sicker people’s higher premiums. This would require substantial new taxes, however, which is presumably a nonstarter in a Republican plan. In any case, it would only make the transfers to older, sicker people more explicit.
The second challenge is more nakedly political: Without a substantial change in Senate procedure, a bill to fully replace the Affordable Care Act, including changes to insurance rules, will require 60 votes. Republicans have only 52, so at least eight Democratic senators would need to be persuaded to go along. This is a much tougher assignment, especially since the administration will already be calling in legislative favors on ongoing confirmations, the debt limit, tax reform and other issues.
The Republicans’ desire to hold an early partisan vote repealing the ACA (through the reconciliation process that requires only a simple majority in the Senate) seems too strong to resist. The repeal will probably be set to become effective in the future, perhaps 2019 or 2020.
This vote will probably be closer than many people think, given the concerns that some moderate Republican senators have expressed about repealing the ACA with no replacement ready. Some far-right Republicans may also balk at anything less than a full immediate repeal. For the White House, however, the closeness of the vote will be a feature rather than a bug, because it will create the impression that the vote is significant.
The repeal legislation will probably include some modest steps toward replacing the ACA, but these will be mostly symbolic measures such as allowing insurance companies to sell across state lines (which by itself would do little to lower people’s premiums). The hard work of a creating comprehensive replacement is then likely to get bogged down in legislative muck.
But the administration can use its expansive waiver authority to allow states to experiment with both Medicaid and the individual insurance markets. As these 50 flowers bloom, President Trump could at some point declare victory and assert that the ACA has been sufficiently reformed.
This approach, whatever its potential substantive shortcomings, provides a major political benefit: The administration would not necessarily own the many problems that inevitably would remain. In response to any particular complaint in a specific state, the administration could simply shrug its shoulders and direct the inquiry to the relevant governor.
This outlook assumes that the Republican leadership in Congress isn’t willing, or lacks the votes, to change the Senate’s traditional rules, and that a comprehensive replacement for the ACA will indeed require 60 votes. If that changes, all bets are off.
This column does not necessarily reflect the opinion of the editorial board or Bloomberg LP and its owners.
To contact the author of this story:
Peter R. Orszag at porszag5@bloomberg.net
To contact the editor responsible for this story:
Mary Duenwald at mduenwald@bloomberg.net

by Alex | Feb 9, 2017 | Health Care Reform
 Trump Order and ACA
Trump Order and ACA
President Trump signed an Executive Order on Jan 20 Minimizing the Economic Burden of the Patient Protection and Affordable Care Act Pending Repeal. As a practical matter, he can’t repeal it “line-by-line on day one” of his Presidency. So he did the next best thing: sign an Executive Order.
While lawmakers work on a repeal and replacement plan, here are 5 things you should know. The executive order will:
- End the individual mandate.
- Expand Medicaid waivers and provide states more flexibility to implement healthcare programs.
- Encourage the creation of interstate insurance markets to “the maximum extent permitted by the law.”
- Remove ACA taxes, including some placed on health insurance and pharmaceutical companies, in addition to waiving PPACA taxes, fees, and penalties.
- Grant leaders of the Department of Health and Human Services (HHS) and other agencies to exercise greater discretion. This includes the ability to waive, defer, or grant an exception to any provision that would impose a fiscal burden on a state or place a financial or regulatory burden (cost, fee tax, penalty) on individuals, families, healthcare providers, and patients.
We will soon know whether the Executive Order is more symbolic or has practical effects. Employers should continue to comply with the provisions in current law, until official guidance provides otherwise.

by Alex | Nov 10, 2016 | Health Care Reform, Obamacare
2017 Election Results and ACA
The 2017 Election Results and ACA is a hot topic creating buzz. With the outcome of the 2016 elections now official, the Republicans will hold the majority in both chambers of Congress and control of the White House beginning in 2017. Our posting CLINTON VS TRUMP ON HEALTHCARE was a general summary of their differences on Healthcare.
Since President-elect Trump ran on a platform of “Replace and Repeal” of the Affordable Care Act (ACA), we anticipate that acting on this campaign promise will be one of the top priorities of the new Trump administration. We anticipate there will be significant disruption for individuals, employers, brokers and carriers across the country.
Republicans will likely need to use the process of Budget Reconciliation to pass legislation through the Senate, given the party did not secure enough seats to control a filibuster-proof supermajority. In other words, the legislation can pass in the Senate with a simple majority vote and not a super majority (which requires 60 votes). Reconciliation can be used to take away some, but not all, of the ACA. It is anticipated that certain provisions of the ACA would be targeted such as Medicaid expansion, the availability of subsidies and premium tax credits in the Marketplace, and the employer and individual mandate. It cannot be used to remove non-budgetary provisions (for example, insurance mandates like “to age 26”). In addition, it is conceivable that a Trump administration may simply direct various federal agencies (such as the Department of Labor) to not enforce certain ACA provisions.
The Republicans have not laid out a specific plan on what will replace the ACA. Generally, the party has supported the existing employer-based system (with some party members calling for limits on the tax exclusion). Based on published white papers on the President-elect Trump’s website, other aspects of a healthcare overhaul plan may include:
- Tax credits for purchasing individual health insurance;
- Expansion of Health Savings Accounts and HighDeductible Health Plans;
- Continuation of the prohibition on pre-existing condition exclusions from health insurance;
- High risk pools;

- Interstate sales of insurance; andMedical malpractice reform.
The process to repeal and replace the ACA will take time and nothing will happen between now and the New Year. Open enrollment is currently underway in the Marketplaces across the country and it is expected that individual policies (and subsidies for lower and middle-income individuals) will be available to enrollees as of January 1, 2017. What is unknown is whether the Trump administration and subsequent legislation will affect the Marketplace and subsidies in mid-2017 or instead phase out this coverage after the 2017 calendar year.
- The employer mandate (for applicable large employers);
- Form 1094-C and 1095-C reporting for CalendarYear 2016;
- Any ACA taxes and fees for self-funded plans to pay directly (such as reinsurance fees); and
- Plan design changes applicable to plan years thatbegin on or after January 1, 2017.
In addition, all other federal law mandates impacting employer health and welfare plans such as ERISA,HIPAA, COBRA, Code Section 125, the Mental Health Parity and Addiction Equity Act, and the Service Contract Act / Davis Bacon and Related Acts are still good law. There has been no indication that these non-ACA laws are targeted for repeal or replacement.
Stay tuned for updates as more information gets released. Sign up for latest news updates. Please contact our team on your 2017 health plan renewal at Millennium Medical Solutions Corp (855)667-4621 for immediate answers.
by Alex | Oct 31, 2016 | family health insurance, Health Care Reform, Health Exchanges, Individual Exchanges, individual health insurance, State Exchanges
2017 Individual Open Enrollment
Everything you need to know ahead of tomorrow’s 2017 Individual Open Enrollment. This Open Enrollment marks the 4th anniversary of Obamacare a.ka. The Affordable Care Act. As a helpful resource, the new NY and NJ rates with important deadlines are listed below. 33 States such as NJ use the healthcare.gov website or at https://medicalsolutionscorp.demo.hcinternal.net/individual/individual/homePage. States such as NY and CT use their own Marketplace – NYS of Health and AccessHealth CT. Importantly, individuals not expecting a subsidy may also apply Off-Exchange which in many case has more options and Insurers.
2017 NY Individual Health Plans
 These rates are for New York City unless otherwise indicated, and for a single person. For a family premium, multiply by 2.85, Husband/Wife
These rates are for New York City unless otherwise indicated, and for a single person. For a family premium, multiply by 2.85, Husband/Wife
multiply by 2.0 and Parent/Children multiply by 1.70. The non single deductibles are out of pocket maximums are doubled. These are for standard plans, which two-thirds of customers enrolled in during 2016.
While deductibles for platinum, gold and silver plans have stayed the same, many bronze plan deductibles have increased 33 percent. That means consumers who purchase a bronze plan — presumably for its lower monthly premium — are paying more out of pocket for their medical costs before their insurance company kicks in a dime. A family of four that purchased a bronze plan will have an $8,000 deductible in 2017, up from $6,000 in 2015. For someone young and relatively healthy, that might be OK, but that person is vulnerable to a very large bill if he or she needs expensive medical care. It’s the platinum plans where New York State really shows itself to be a national outlier. Roughly 18 percent of New Yorkers chose a platinum plan in 2016, compared to 2 percent across the nation, according to the Kaiser Family Foundation.
Here are the 2017 rates:
2017-nys-marketplace-rates-1
2017 NJ Individual Health Plans
NJ Dept of Banking and Insurance posted the 2017 NJ individual health plans Monday. Only two carriers will offer plans on the state’s Obamacare marketplace next year: Horizon Blue Cross Blue Shield of New Jersey and AmeriHealth.
Additional insurers are participating off-exchange or outside the Marketplace. Examples: Aetna, CIGNA and Oxford. There are additional 20 plan options available off exchange. A notable new entrant, Health Republic of NJ, will no longer be available for 2017. See – Health Republic NJ Shutting Down.
Here are the 2017 rates:
2017-new-jersey-individual-health-benefits-plans-and-rates
2017 Individual Open Enrollment Deadlines
- November 1, 2016: Open Enrollment starts — first day you can enroll in a 2017 insurance plan through the Health Insurance Marketplace. Coverage can start as soon as January 1, 2016.
- December 15, 2016: Last day to enroll in or change plans for new coverage to start January 1, 2017.
- January 1, 2017: 2017 coverage starts for those who enroll or change plans by December 15.
- January 15, 2017: Last day to enroll in or change plans for new coverage to start February 1, 2017
- January 31, 2017: 2016 Open Enrollment ends. Enrollments or changes between January 16 and January 31 take effect March 1, 2017.
If you don’t enroll in a 2016 health insurance plan by January 31, 2017, you can’t enroll in a health insurance plan for 2016 unless you qualify for a Marketplace Special Enrollment Period.
Penalty: The uninsured penalty rises to $695 or 2.5% of your income, whichever is higher.
Coverage start dates
If you enroll before the 15th of any month, your coverage starts the first day of the next month. If you enroll after the 15th of the month, you’ll have to wait until the month after that for your coverage to start. So, for example, if you enroll on January 16, your coverage would start on March 1.
Enroll using our online comparison shopping tool for both on and off-Exchange Marketplace to be released next week. Email us or Contact us at (855)667-4621.

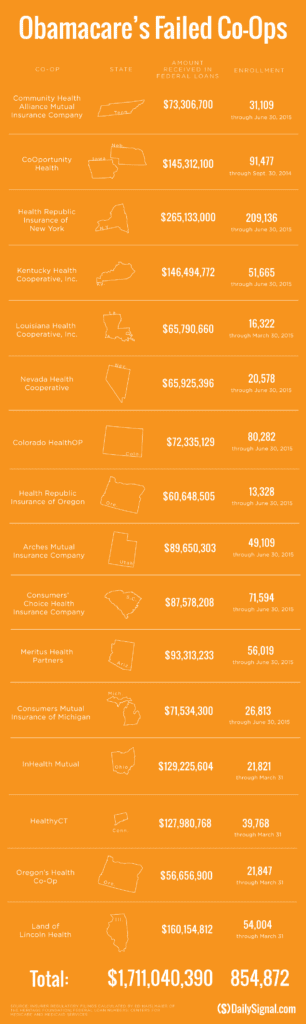
by Alex | Sep 13, 2016 | Health Care Reform, Health Exchanges, Obamacare, regional health insurance co-ops, State Exchanges
Health Republic NJ Shutting Down

Health Republic NJ Shutting Down
In yesterday’s surprise announcement, NJ regulators will be shutting down Health republic NJ for 2017 “because of its hazardous financial condition”. This marks the demise of the second Metro area healthcare co-op with the same name-sake Health Republic but different managed healthcare co-op, see Health Republic NY Shutting Down Nov 30.
Since Obamacare’s rollout in the fall of 2013, 16 co-ops that launched with money from the federal government have collapsed. Now, just six co-ops—Wisconsin’s Common Ground Healthcare Cooperative; Maryland’s Evergreen Health Cooperative; Maine Community Health Options; Massachusetts’ Minuteman Health; Montana Health Cooperative; and New Mexico Health Connections—remain.
In a bizarre twist of fate or unintended Affordable Care Act design flaw small affordable startups not only have to gain new client footholds but also support large
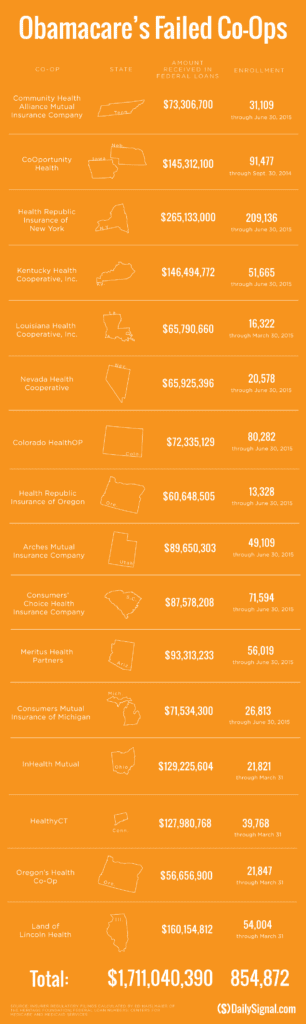
established companies “with sicker patients”. Start-ups, by contrast, with much lower rate of diagnosed sick patients essentially pay into this tax. This tax is part of the risk adjustment program intended to stabilize Insurers who took on sicker patients and spread this risk. While some correctly blame too low pricing and some miscalculated business decision-making the inherent extra tax doomed the majority of the original 16 co-ops.
Health Republic in fact grew steadily and made money the first 9 months of 2015. However, HRNJ lost 17.6 million end of 2015 and is choking off at this $46.3 million payment to the government through the risk adjustment program. This is considered one of the 3 R’s of the reinsurance program – risk corridor, reinsurance and risk adjustment that were intended to level the playing field. The first “R”—“reinsurance”—subsidizes insurers that attract individual customers who rack up particularly high medical bills. The second—“risk adjustment”—requires insurers with low-cost patients to make payments to plans that share the benefits with those who insured higher-cost ones. And the third, called “risk corridors,” is a program to subsidize health plans whose total medical expenses for all their Obamacare customers overshoot a target amount.
The co-ops received less money than they initially anticipated last year under Obamacare’s risk corridor program, which resulted in the collapse of at least five co-ops and a $5 billion class action lawsuit
filed by 6 state’s co-ops – ” Oregon-based insurer Moda Health Plan Inc., Blue Cross Blue Shield of North Carolina, Pittsburgh-based Highmark Inc., and the failed CoOportunity Health, which was based in West Des Moines, Iowa, and Health Republic Insurance Co. of Oregon, which was based in Lake Oswego.”
From Politico’s “Obamacare’s sinking safety net”:
“The risk corridor program, however, has been an unmitigated debacle. In December 2014, the Republican Congress voted to prohibit the Obama administration from spending any money on the program, decrying it as a bailout for the insurance companies. Sen. Marco Rubio, then thought to be a leading GOP presidential contender for 2016, was particularly vocal in pillorying the program.
Unlike all those symbolic “repeal Obamacare” votes, Congress actually succeeded in blocking those risk corridor payments, and it hit Obamacare hard. Insurers filed claims seeking $2.9 billion, but under the limits imposed by the GOP there was less than $400 million available to make good on those payments. The end result: insurers initially received only 12.6 cents for each dollar they had counted on. Many of the new Obamacare co-op plans that went out of business blamed their collapse in part on the fact that they’d been counting on the full payments to keep them solvent.”
Regrettably, in a Presidential year no one wants to touch this burning hot potato. Perhaps NJ’s handling of this pressure cooker and taking 2017 off may be the best course of action after all.
9/16/16 Addendum:
As of Monday, September 19, 2016, the portal for Health Republic Insurance will be shut down, as they are no longer accepting new business for the year.
The New Jersey State Department of Banking and Insurance has also provided a list of FAQs related to the shutdown and how it affects individuals, small employers, brokers and providers. For more information, click here.
As always, our team is here to assist you and to help you grow your business.






 These rates are for New York City unless otherwise indicated, and for a single person. For a family premium, multiply by 2.85, Husband/Wife
These rates are for New York City unless otherwise indicated, and for a single person. For a family premium, multiply by 2.85, Husband/Wife

 established companies “with sicker patients”. Start-ups, by contrast, with much lower rate of diagnosed sick patients essentially pay into this tax. This tax is part of the risk adjustment program intended to stabilize Insurers who took on sicker patients and spread this risk. While some correctly blame too low pricing and some miscalculated business decision-making the inherent extra tax doomed the majority of the original 16 co-ops.
established companies “with sicker patients”. Start-ups, by contrast, with much lower rate of diagnosed sick patients essentially pay into this tax. This tax is part of the risk adjustment program intended to stabilize Insurers who took on sicker patients and spread this risk. While some correctly blame too low pricing and some miscalculated business decision-making the inherent extra tax doomed the majority of the original 16 co-ops.