by admin | Feb 3, 2014 | Health Care Reform, Health Exchanges, Individual Exchanges, PPACA, SHOP Exchanges, State Exchanges
Licensed Brokers vs Navigators
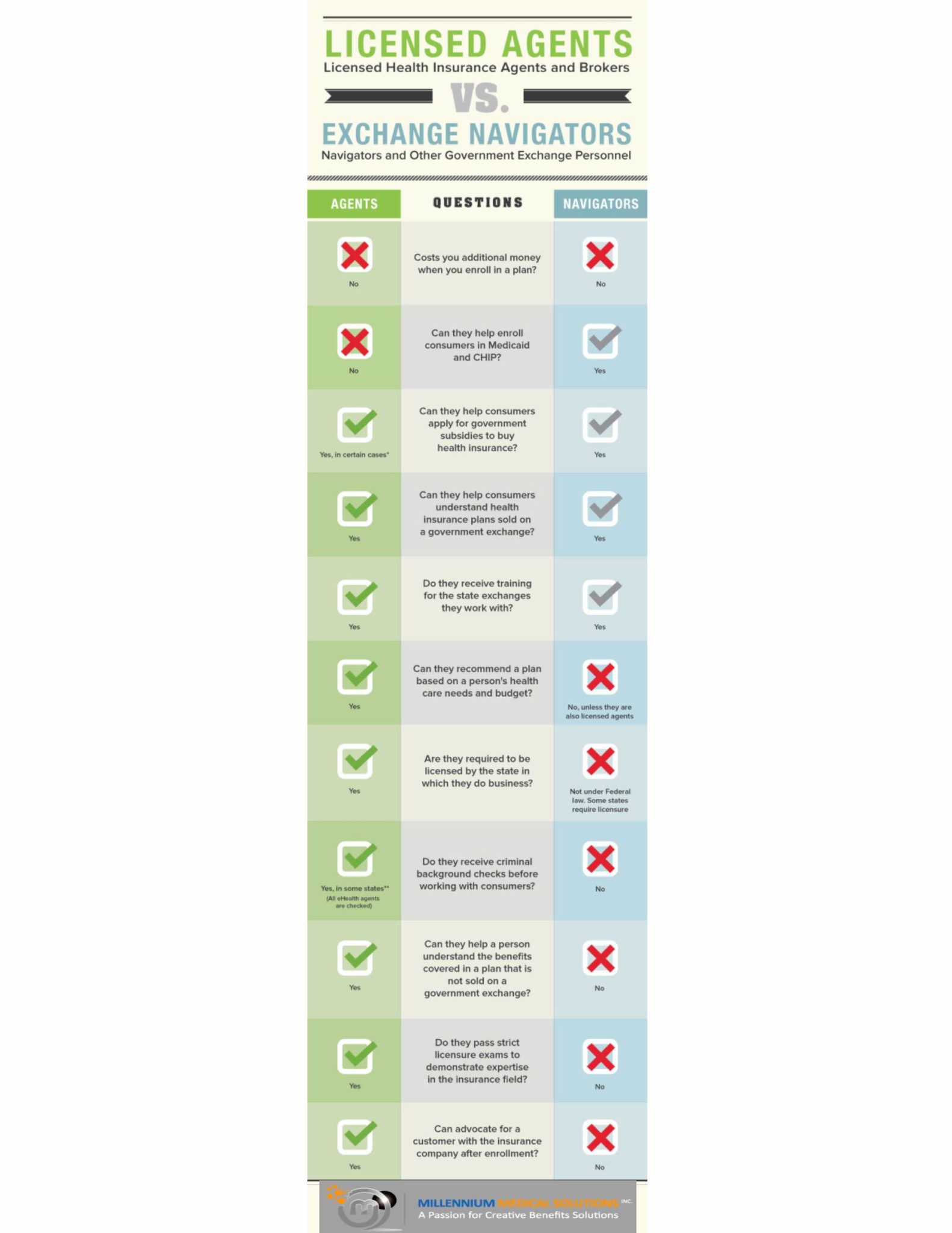
With less than 45 days before the first Affordable Care Act Open Enrollment set to end its important to understand the role of both Brokers and Navigators. The Patient Protection and Affordable Care Act (PPACA) requires States to establish a “Navigator” Program to help educate consumers about Health Exchange marketplace. With the new health insurance exchanges a broker can act either as a traditional broker or a navigator (but not both). The info-graph below illustrates how navigators will differ from brokers.
 Specifically, agents and brokers play a vital role in the developing health insurance exchanges nation wide. As the individuals with the education and expertise to advise and help select health insurance products for families and businesses large and small, health insurance agents, brokers and consultants occupy a unique place in the health care coverage system.
Specifically, agents and brokers play a vital role in the developing health insurance exchanges nation wide. As the individuals with the education and expertise to advise and help select health insurance products for families and businesses large and small, health insurance agents, brokers and consultants occupy a unique place in the health care coverage system.
We educate consumers on their health care coverage choices, help them select the most appropriate plans for their specific needs, and serve as their advocate if problems should arise. Subject to strict state licensing laws and education requirements, agents, brokers and consultants are critical to not only the health insurance enrollment process, but also in serving the healthinsurance coverage needs of individuals and employers after the point of sale.
Benefit specialists design benefit plans, explain coordination issues of public and private benefits to individuals and employees, and solve complex claims and billing issues. We help design and implement cutting-edge health promotion and wellness programs and help our clients comply with state and federal laws like newly enacted PPACA, HIPAA, COBRA and ERISA.
Professional agents, brokers and consultants continue to assist individuals and small businesses with their coverage needs long after the point of sale. Whereas a travel agent is finished with a client after the travel is completed, benefit specialists continues to serve as compliance experts, health and wellness promoters and the prominent contact for complex claims and billing issues. Health insurance coverage is a longstanding commitment for American consumers and often requires guidance from benefit specialists when dealing with a complex healthcare system.
For more information regarding both Exchanges – Individual Exchanges or SHOP please contact our team at Millennium Medical Solutions Corp (855)667-4621. We work in coordination with Navigators to assist with medicaid, CHIP Child Health Plus, Family Health Plus and Medicare Dual Eligibles. We have Spanish, Russian, and Hebrew speakers available. Quotes can also be viewed on our site. by admin | Aug 7, 2009 | COBRA, Dependent Coverage, family health insurance, group health insurance, individual health insurance, latest health insurance news, NY News
As expected, Governor David Paterson has signed 3 of his healthcare reform proposals into law, to wit:
S.5471 (Breslin) / A.8400 (Peoples) – extends state mini-COBRA from 18 to 36 months. Effective date is July 1, 2009 and shall apply to all policies and contracts of insurance issued, renewed, modified, altered or amended on or after such date.
S.6030 (Breslin) / A.9038 (Morelle) – allows for dependent care coverage of children up to 29 years of age. Effective date is September 1, 2009 and shall apply to all policies and contracts of insurance issued, renewed, modified, altered or amended on or after such date.
S.5472-A (Breslin) / A.8402-A (Morelle) – HMO reform act. Various effective dates depending upon the specific provision of the bill.
Here’s a link to the Governor’s Press Release announcing the same:
Article in Newsday – “New state law eases medical coverage for 20-somethings”
![Legislative Alert: Stimulus Package/COBRA UPDATE]()
by admin | Mar 9, 2009 | COBRA, healthcare
 The American Resources and Recovery and Reinvestment Act of 2009 was signed into law by President Obama February 17th. Under the Act, certain individuals who are eligible for COBRA continuation health coverage, or similar coverage under State law, may receive a subsidy for 65 percent of the premiums for themselves and their families for up to nine months.
The American Resources and Recovery and Reinvestment Act of 2009 was signed into law by President Obama February 17th. Under the Act, certain individuals who are eligible for COBRA continuation health coverage, or similar coverage under State law, may receive a subsidy for 65 percent of the premiums for themselves and their families for up to nine months.
Click on the link below for detailed information on the American Recovery and Reinvestment Act of 2009 which went into effect February 17, 2009
http://www.dol.gov/ebsa/cobra.html
These individuals are required to pay only 35 percent of the premium.
The employer may recover the subsidy provided to assistance-eligible individuals by taking the subsidy amount as a credit on its quarterly employment tax return. The employer may provide the subsidy – and take the credit on its employment tax return – only after it has received the 35 percent premium payment from the individual.
To qualify, a worker must have been involuntarily separated between Sept. 1, 2008, and Dec. 31, 2009. Workers who lost their jobs between Sept. 1, 2008, and enactment, but failed to initially elect COBRA because it was unaffordable, get an additional 60 days to elect COBRA and receive the subsidy.
This subsidy phases out for individuals whose modified adjusted gross income exceeds $125,000, or $250,000 for those filing joint returns. Taxpayers with modified adjusted gross income exceeding $145,000, or $290,000 for those filing joint returns, do not qualify for the subsidy.
On February 26, the Internal Revenue Service released its first round of information for employers to use in administering the new subsidy program. Included are the subsidy reporting form, instructions and a very detailed questions-and-answers piece. The Department of Labor is still working on model notices and other guidance for release by March 17.
 Specifically, agents and brokers play a vital role in the developing health insurance exchanges nation wide. As the individuals with the education and expertise to advise and help select health insurance products for families and businesses large and small, health insurance agents, brokers and consultants occupy a unique place in the health care coverage system.
Specifically, agents and brokers play a vital role in the developing health insurance exchanges nation wide. As the individuals with the education and expertise to advise and help select health insurance products for families and businesses large and small, health insurance agents, brokers and consultants occupy a unique place in the health care coverage system.
 The American Resources and Recovery and Reinvestment Act of 2009 was signed into law by President Obama February 17th. Under the Act, certain individuals who are eligible for COBRA continuation health coverage, or similar coverage under State law, may receive a subsidy for 65 percent of the premiums for themselves and their families for up to nine months.
The American Resources and Recovery and Reinvestment Act of 2009 was signed into law by President Obama February 17th. Under the Act, certain individuals who are eligible for COBRA continuation health coverage, or similar coverage under State law, may receive a subsidy for 65 percent of the premiums for themselves and their families for up to nine months.