
Health Advocate
Health Advocate
Health Advocate is a concierge service partner provided by Millennium Medical Solutions Corp. It can help you and your eligible family members connect to your benefits, resolve healthcare and insurance-related issues, improve your health and balance your work and life. For more information, check out the One Call Number for all your healthcare needs.
Health Advocate also offers workshops to help you quit smoking, lose weight and more! Log in to your member portal to check out the additional resources! Check out any of the following wellness resources by clicking the links below:
Don’t forget to also connect with their blog for more health resources by clicking here or you can peak through the Health Advocate newsletter archives at the links at the bottom of this page.
Looking for something else? Learn more about what Health Advocate has to offer you by clicking here: health advocate
Access Your Member Website
Log on to the website: HealthAdvocate.com/members
• Download member essentials
• Access your Wellness program
• Reach EAP and Work/Life services
…and much more
Contacting Health Advocate
Call: 866.799.2691
Email: answers@HealthAdvocate.com

Which Chocolate Is Best for Your Heart?
Which Chocolate Is Best for Your Heart?
Dark, Milk or White – Which Chocolate Is Best for Your Heart? (Infographic)
From our wellness partner, Cleveland Clinic
Chocolate is good for blood flow, which means it’s good for your heart. But not all chocolate is created equal. Find out about the healthy antioxidants and what else is inside so you can make the best choice of chocolate for your heart health.

Employer Premium Reimbursement Accounts
On November 6th, the government issued their 22nd set of FAQs on ACA. This FAQ makes it clear that an employer cannot offer employees cash to reimburse the purchase of an individual policy.
Such an arrangement may be subject to a $100/day excise tax per applicable employee (which is $36,500 per year, per employee tax).
FAQs about Affordable Care Act Implementation (Part XXII)
November 6, 2014
Set out below are additional Frequently Asked Questions (FAQs) regarding implementation of the Affordable Care Act. These FAQs have been prepared jointly by the Departments of Labor (DOL), Health and Human Services (HHS), and the Treasury (collectively, the Departments). Like previously issued FAQs (available at http://www.dol.gov/ebsa/healthreform/ and http://www.cms.gov/cciio/resources/fact-sheets-and-faqs/index.html), these FAQs answer questions from stakeholders to help people understand the new law and benefit from it, as intended.
Compliance of Premium Reimbursement Arrangements
On September 13, 2013, DOL and the Treasury published guidance on the application of the market reforms and other provisions of the Affordable Care Act to health reimbursement arrangements (HRAs), certain health flexible spending arrangements (health FSAs) and certain other employer health care arrangements.(1) HHS issued contemporaneous guidance to reflect that HHS concurs in the application of the laws under its jurisdiction as set forth in the DOL and Treasury Department guidance.(2) Subsequently, on May 13, 2014, two FAQs were made available on the IRS website addressing employer health care arrangements.(3)
The Departments’ prior guidance explains that employer health care arrangements, such as HRAs and employer payment plans, are group health plans that typically consist of a promise by an employer(4) to reimburse medical expenses up to a certain amount. The Departments’ guidance clarifies that such arrangements are subject to the group market reform provisions of the Affordable Care Act, including the prohibition on annual limits under Public Health Service Act (PHS Act) section 2711 and the requirement to provide certain preventive services without cost sharing under PHS Act section 2713.(5) The Departments’ guidance further clarifies that such employer health care arrangements will not violate these market reform provisions when integrated with a group health plan that complies with such provisions. However, an employer health care arrangement cannot be integrated with individual market policies to satisfy the market reforms. Consequently, such an arrangement may be subject to penalties, including excise taxes under section 4980D of the Internal Revenue Code (Code).
Q1: My employer offers employees cash to reimburse the purchase of an individual market policy. Does this arrangement comply with the market reforms?
No. If the employer uses an arrangement that provides cash reimbursement for the purchase of an individual market policy, the employer’s payment arrangement is part of a plan, fund, or other arrangement established or maintained for the purpose of providing medical care to employees, without regard to whether the employer treats the money as pre-tax or post-tax to the employee. Therefore, the arrangement is group health plan coverage within the meaning of Code section 9832(a), Employee Retirement Income Security Act (ERISA) section 733(a) and PHS Act section 2791(a), and is subject to the market reform provisions of the Affordable Care Act applicable to group health plans. Such employer health care arrangements cannot be integrated with individual market policies to satisfy the market reforms and, therefore, will violate PHS Act sections 2711 and 2713, among other provisions, which can trigger penalties such as excise taxes under section 4980D of the Code. Under the Departments’ prior published guidance, the cash arrangement fails to comply with the market reforms because the cash payment cannot be integrated with an individual market policy.(6)
Q2: My employer offers employees with high claims risk a choice between enrollment in its standard group health plan or cash. Does this comply with the market reforms?
No. PHS Act section 2705,(7) which was incorporated by reference into ERISA section 715 and Code section 9815, as well as the nondiscrimination provisions of ERISA section 702 and Code section 9802 originally added by the Health Insurance Portability and Accountability Act (HIPAA), prohibit discrimination based on one or more health factors. Offering, only to employees with a high claims risk, a choice between enrollment in the standard group health plan or cash, constitutes such discrimination. While the Departments’ regulations implementing this provision(8) permit more favorable rules for eligibility or reduced premiums or contributions based on an adverse health factor (sometimes referred to as benign discrimination), in the Departments’ view, cash-or-coverage arrangements offered only to employees with a high claims risk are not permissible benign discrimination. Accordingly, such arrangements will violate the nondiscrimination provisions, regardless of whether (1) the cash payment is treated by the employer as pre-tax or post-tax to the employee, (2) the employer is involved in the selection or purchase of any individual market product, or (3) the employee obtains any individual health insurance.
Such offers fail to qualify as benign discrimination for two reasons. First, if an employer offers a choice of additional cash or enrollment in the employer’s plan to a high-claims-risk employee, the opt-out offer does not reduce the amount charged to the employee with the adverse health factor. Rather, the employer’s offer of cash to a high-claims-risk employee who opts out of the employer’s plan effectively increases the premium or contribution the employer’s plan requires the employee to pay for coverage under the plan because, unlike other similarly situated individuals, the high-claims-risk employee must accept the cost of forgoing the cash in order to elect plan coverage. For example, if the employer’s group health plan requires all employees to pay $2,500 toward the cost of employee-only coverage under the plan, but the employer offers a high-claims-risk employee $10,000 in additional compensation if the employee declines the coverage, for purposes of discrimination analysis, the effective required contribution by that high-claims-risk employee for plan coverage is $12,500 – that is, the $2,500 required employee contribution for employee-only coverage under the employer’s plan plus the $10,000 of additional compensation that the employee would forgo by enrolling in the plan. Because a high-claims-risk employee must effectively contribute more to participate in the group health plan, the arrangement violates the rule that a group health plan may not on the basis of a health factor require any individual (as a condition of enrollment) to pay a premium or contribution which is greater than the premium or contribution for a similarly situated individual enrolled in the plan.
Second, the Departments’ regulations generally permit providing, based on an adverse health factor, enhancements to eligibility for coverage under the plan itself but not cash as an alternative to the plan. In particular, the regulations permit providing plan eligibility criteria that offer extended coverage within the plan and subsidization of the cost of coverage within the plan based on an adverse health factor.(9) An example in the Departments’ regulations illustrates that a plan may have an eligibility provision that provides coverage to disabled dependent children beyond the age at which non-disabled dependent children become ineligible for coverage.(10) Another example in the regulations illustrates that a plan may provide coverage free of charge to disabled employees, while other employees pay a participant contribution towards coverage.(11) However, in the Departments’ view, providing cash as an alternative to health coverage for individuals with adverse health factors is an eligibility rule that discourages participation in the group health plan. This type of arrangement differentiates based on a health factor and is outside the scope of the Departments’ regulations on benign discrimination, which permit only discrimination that helps individuals with adverse health factors to participate in the health coverage being offered to other plan participants. The Departments intend to initiate rulemaking in the near future to clarify the scope of the benign discrimination provisions.
Finally, because the choice between taxable cash and a tax-favored qualified benefit (the election of coverage under the group health plan) is required to be a Code section 125 cafeteria plan, imposing an effective additional cost to elect coverage under the group health plan could, depending on the facts and circumstances, also result in discrimination in favor of highly compensated individuals in violation of the Code section 125 cafeteria plan nondiscrimination rules.
Q3: A vendor markets a product to employers claiming that employers can cancel their group policies, set up a Code section 105 reimbursement plan that works with health insurance brokers or agents to help employees select individual insurance policies, and allow eligible employees to access the premium tax credits for Marketplace coverage. Is this permissible?
No. The Departments have been informed that some vendors are marketing such products. However, these arrangements are problematic for several reasons. First, the arrangements described in this Q3 are themselves group health plans and, therefore, employees participating in such arrangements are ineligible for premium tax credits (or cost-sharing reductions) for Marketplace coverage. The mere fact that the employer does not get involved with an employee’s individual selection or purchase of an individual health insurance policy does not prevent the arrangement from being a group health plan. DOL guidance indicates that the existence of a group health plan is based on many facts and circumstances, including the employer’s involvement in the overall scheme and the absence of an unfettered right by the employee to receive the employer contributions in cash.(12)
Second, as explained in DOL Technical Release 2013-03, IRS Notice 2013-54, and the two IRS FAQs addressing employer health care arrangements referenced earlier, such arrangements are subject to the market reform provisions of the Affordable Care Act, including the PHS Act section 2711 prohibition on annual limits and the PHS Act 2713 requirement to provide certain preventive services without cost sharing. Such employer health care arrangements cannot be integrated with individual market policies to satisfy the market reforms and, therefore, will violate PHS Act sections 2711 and 2713, among other provisions, which can trigger penalties such as excise taxes under section 4980D of the Code.
Footnotes
1. See DOL Technical Release 2013-03, available at http://www.dol.gov/ebsa/newsroom/tr13-03.html, and IRS Notice 2013-54, available at http://www.irs.gov/pub/irs-drop/n-13-54.pdf.
2. See Insurance Standards Bulletin, Application of Affordable Care Act Provisions to Certain Healthcare Arrangements, September 16, 2013, available at https://www.cms.gov/CCIIO/Resources/Regulations-and-Guidance/Downloads/cms-hra-notice-9-16-2013.pdf.
3. Available at: www.irs.gov/uac/Newsroom/Employer-Health-Care-Arrangements.
4. These arrangements may be sponsored by an employer, an employee organization, or both. For simplicity, this section of the FAQs refers to employers. However, this guidance is equally applicable to HRAs sponsored by employee organizations, or jointly by employers and employee organizations.
5. Section 1001 of the Affordable Care Act added new PHS Act §§ 2711-2719. Section 1563 of the Affordable Care Act (as amended by Affordable Care Act § 10107(b)) added Code § 9815(a) and ERISA § 715(a) to incorporate the provisions of part A of title XXVII of the PHS Act into the Code and ERISA, and to make them applicable to group health plans and health insurance issuers providing health insurance coverage in connection with group health plans. The PHS Act sections incorporated by these references are sections 2701 through 2728. Accordingly, these referenced PHS Act sections (i.e., the market reforms) are subject to shared interpretive jurisdiction by the Departments.
6. See DOL Technical Release 2013-03, available at http://www.dol.gov/ebsa/newsroom/tr13-03.html, and IRS Notice 2013-54, available at http://www.irs.gov/pub/irs-drop/n-13-54.pdf. See also Insurance Standards Bulletin, Application of Affordable Care Act Provisions to Certain Healthcare Arrangements, September 16, 2013, available at https://www.cms.gov/CCIIO/Resources/Regulations-and-Guidance/Downloads/cms-hra-notice-9-16-2013.pdf.
7. Prior to the enactment of the Affordable Care Act, Titles I and IV of the Health Insurance Portability and Accountability Act of 1996 (HIPAA), Public Law 104-191, added section 9802 of the Code, section 702 of ERISA, and section 2702 of the PHS Act (HIPAA nondiscrimination and wellness provisions). Affordable Care Act section 1201 also moved those provisions in the PHS Act from section 2702 to section 2705.
8. 26 CFR 54.9802-1 (g); 29 CFR 2590.702(g);146.121(g).
9. 26 CFR 54.9802-1 (g)(1)(i); 29 CFR 2590.702(g)(1)(i);146.121(g)(1)(i).
10. 26 CFR 54.9802-1 (g)(1)(ii), Example 1; 29 CFR 2590.702(g)(1)(ii), Example 1;146.121(g)(1)(ii), Example 1.
11. 26 CFR 54.9802-1 (g)(2)(ii), Example; 29 CFR 2590.702(g)(2)(ii), Example;146.121(g)(2)(ii), Example.
12. See 29 CFR 2510.3-1(j).
Click here for printer friendly version.

NATIONAL IMMUNIZATION AWARENESS MONTH
NATIONAL IMMUNIZATION AWARENESS MONTH
Immunizations are one of the top ten public health accomplishments of the twentieth century according to the CDCP (Center for Disease Control and Prevention).
 Talk with your health care provider, not just about childhood vaccines, but for adults also. This knowledge may help prevent illness and outbreaks due to vaccine preventable diseases. Vaccines are recommended throughout your lifetime. They are an important step in protecting against serious and sometimes deadly diseases.
Talk with your health care provider, not just about childhood vaccines, but for adults also. This knowledge may help prevent illness and outbreaks due to vaccine preventable diseases. Vaccines are recommended throughout your lifetime. They are an important step in protecting against serious and sometimes deadly diseases.
Vaccines are proven to protect children from fourteen serious diseases before the age of two. Adolescence from cancer caused by certain types of HPV, young adults from meningitis and people of all ages from flu, as well as, the aging population from various illnesses.
New York State Immunization Requirements for School Entrance:Attendance1 Local States already requires specific vaccines for public school attendance. There is an assistance program offered, by the Pennsylvania department of health, to obtain vaccinations through federally funded “Vaccines for Children”, providing access to immunizations to low income, underinsured children through age 18. Uninsured children regardless of income are eligible for the Children’s health insurance program. Adults are encouraged also to review their immunizations with their physician, also checked with your individual insurance plan for coverage of adult immunizations, for the specific vaccines covered under your plan.
Please refer to the “CDC” (Center for Disease Control) website for further information on types of immunizations suggested for pre-school, adolescents and adults. http://www.cdc.gov/vaccines/schedules/index.html
Please note: This article is for informational purposes only and is not meant to replace the advice of a medical professional. To schedule your Employer day of wellness & flu vaccinations call us (855) 667-4621.

Apple Watch Wearable Workout
Apple Watch Wearable Workout
Alas, Apple has finally unveiled the stylish Apple Watch at today’s celebrated annual presentation. This anticipated product has been talked about so long that its easy to forget its a ground-breaking invention. This gadget is as much a story about fashion and health wellness as tech.
Not surprisingly , the integration of health sensors is a key feature. While the exact specs were not released we do know it will measure heart rate, track steps, milage, calories and sleep, and its GPS system will synch with iPhone. The watch is also designed to “learn” about the wearer, suggesting fitness goals. Apple has developed two different apps that should draw in both gym rats and casual movers. Third Party apps are expected to follow.
This will not be the first wearable workout device. The real estate for your body by fitness companies has been converging but there is nothing arguably this aesthetically beautiful, comprehensively functional and scalable. It will be interesting to see how these wearable devices AKA “Fitbit” is incorporated into work wellness programs. This occupational health was covered in prior blog Wearable Workout at Work:
“Employers incentivizing fitness by lowering lower insurance premiums in exchange for wearing fitness tracking bracelets. Bloomberg reports that BP Plc drive for occupational wellness offered an employee’s spouse the option “to wear a fitness-tracking bracelet from FitBit Inc. to earn points toward cheaper health insurance,” which is “an example of how companies, facing rising health expenses, are increasingly buying or subsidizing fitness-tracking devices to encourage employees and their dependents to be more fit……..UnitedHealth Group Inc. (UNH), Humana Inc. (HUM), Cigna Corp. (CI) and Highmark Inc. have developed similar programs, in which “consumers wear the device and the activity data is uploaded to an online system so it can be verified to give a person their reward.” The article notes, however, that “the moves also let employers and insurers gather more data about people’s lives, raising questions from privacy advocates,” one of whom notes that “when financial incentives are involved, Dixon said it forces employees’ hands and narrows the question of whether or not they should participate.”
The catch? The price tag of $349, unknown battery life and oh yea it only works with the new iPhone 6. Nevertheless, I must of course order one for myself for occupational reasons as part of wellness studies and future articles.
Please contact us on setting up a wellness & fitness program for your business at (855) 667+4621. For MMS Corp previous blogs on wellness, click here. Please contact us on wellness initiatives for your business at (855) 667+4621.

Wearable Workout at Work
Wearable Workout at Work

Fitness Tracking Bracelet
Employers incentivizing fitness by lowering lower insurance premiums in exchange for wearing fitness tracking bracelets. Bloomberg reports that BP Plc drive for occupational wellness offered an employee’s spouse the option “to wear a fitness-tracking bracelet from FitBit Inc. to earn points toward cheaper health insurance,” which is “an example of how companies, facing rising health expenses, are increasingly buying or subsidizing fitness-tracking devices to encourage employees and their dependents to be more fit.
” The article notes that UnitedHealth Group Inc. (UNH), Humana Inc. (HUM), Cigna Corp. (CI) and Highmark Inc. have developed similar programs, in which “consumers wear the device and the activity data is uploaded to an online system so it can be verified to give a person their reward.” The article notes, however, that “the moves also let employers and insurers gather more data about people’s lives, raising questions from privacy advocates,” one of whom notes that “when financial incentives are involved, Dixon said it forces employees’ hands and narrows the question of whether or not they should participate.”
Original Article:
http://www.bloomberg.com/news/2014-08-21/wear-this-device-so-the-boss-knows-you-re-losing-weight.html
Wear This Device So the Boss Knows You’re Losing Weight
To fight rising medical costs, oil company BP Plc (BP) last year offered Cory Slagle — a 260-pound former football lineman — an unusual way to trim $1,200 from his annual insurance bill.
One option was to wear a fitness-tracking bracelet from Fitbit Inc. to earn points toward cheaper health insurance. With the gadget, the 51-year-old walked more than 1 million steps over several months, wirelessly logging the activity on the device. Twelve months later, Slagle has added to his new exercise regimen by trading burgers for salads and soda for water, dropping 70 pounds (31.8 kilograms) and 10 pant sizes in the process.
“I can see my toes now,” said Slagle, a middle-school administrator whose wife, Kristi, works for BP in Houston. The company’s program, he said, is “pushing me to get off the couch and make the right decisions.”
Slagle’s wife is thrilled with his thinner frame — as is BP. His once-high blood pressure and cholesterol are now in a normal range, significantly lowering BP’s risk of covering treatments related to heart trouble or other medical problems.
Slagle’s experience is an example of how companies, facing rising health expenses, are increasingly buying or subsidizing fitness-tracking devices to encourage employees and their dependents to be more fit. The tactic may reduce corporate health-care costs by encouraging healthier lifestyles, even as companies must overcome a creepy factor and concerns from privacy advocates that employers are prying too deeply into workers’ personal lives.

Cory Slagle wore a fitness-tracking bracelet from FitBit Inc. to earn points toward… Read More
Insurers Too
Apart from BP, insurers includingUnitedHealth Group Inc. (UNH),Humana Inc. (HUM), Cigna Corp. (CI) and Highmark Inc. have also created programs to integrate wearable gadgets into their policies. The aim is to get people more invested in taking care of themselves. Consumers wear the device and the activity data is uploaded to an online system so it can be verified to give a person their reward.
“What employers want is the person to take an active role in their health,” said Dee Brock, who has incorporated wearable devices into wellness programs for Pittsburgh-based HighMark.
Privacy Flags
The adoption of wearable devices by companies and insurers is increasing as spending on corporate wellness incentives has doubled to $594 per employee since 2009, according to a study by Fidelity Investments and National Business Group on Health. Technology is creating new forms of wellness programs to measure whether employees are making improvements, similar to a trend in the car-insurance industry where drivers who put a monitoring sensor on their vehicle can earn lower rates based on how well they are driving, instead of their driving history.

Cory Slagle lost 70 pounds after starting to wear a FitBit given to him by energy…Read More
Yet the moves also let employers and insurers gather more data about people’s lives, raising questions from privacy advocates. Wearable gadgets are advancing beyond tracking steps, with sensors to monitor heart rates, glucose levels, body temperature and other functions.
“The focus on preventive health at the expense of privacy is dangerous,” said Pam Dixon, founder of the World Privacy Forum in San Diego, which focuses on health privacy issues. “Right now it’s tracking steps per day, and the reach isn’t that far with these devices, but in time it will be quite sophisticated.”
When financial incentives are involved, Dixon said it forces employees’ hands and narrows the question of whether or not they should participate. The gathering of health data also opens the door for people to eventually be charged more or less based on the information, she said.
Security Requirements
These are among the ethical questions still to be addressed about the appropriateness of companies tracking the physical activity of employees, said Harry Wang, a researcher for Parks Associates who has been studying the market. With wearable devices, collecting more sensitive information is likely to bring tougher government oversight, he said.
“There will be high levels of privacy, security and compliance requirements,” Wang said. “There will be high expectations from consumers about how the data will be used.”
Companies and insurers said they protect the privacy of people using wearable gadgets, and comply with federal laws that prevent employers from seeing certain health information about employees without consent. The wearable programs are voluntary and often administered by third-party vendors like StayWell, which works with BP.
Aggregated Only
As part of the BP program, employees who use a Fitbit to log 1 million steps earn half of the 1,000 points needed each year to qualify for lower co-pays, deductibles and out-of-pocket health expenses. BP bought 25,000 Fitbit devices for North American employees, including those at refineries and drilling rigs. Points can also be earned by getting an annual physical, taking an online health class and other initiatives.
“We think the device is easy to use, gets people aware of how little they are walking and helps trigger people to get active,” said Karl Dalal, director of health and wellness benefits at BP. “BP doesn’t see any of the data except in the aggregate.”
The market for wearable devices is small — about 2 percent of the 1 billion smartphones shipped globally last year — so creating interest from employers and insurance companies is key to growth. Some 22 million fitness-tracking devices will be sold this year, and 66 million by 2018, with about a third coming from corporate-wellness programs, according to Parks Associates. The incentives an employer or insurance company can offer is a way to keep people using the gadget, instead of throwing it in a drawer once the novelty wears off.
Targeting Businesses
Under the Affordable Care Act, the new national health-care law, companies can spend as much as 30 percent of annual insurance premiums on rewards for healthy behavior.
Technology companies are taking note. Apple Inc. (AAPL), which has new health-tracking software called HealthKit that will be released this year and is said to be developing its own wearable device, has talked with UnitedHealth, the biggest U.S. insurer, and Humana, about its health initiatives, executives at the insurance providers said. The companies wouldn’t provide specifics about the conversations. Apple declined to comment.
Fitbit has a sales force dedicated to pitching employers and insurance companies, and touts software to make it easier to log the activity of workers, down to specific individuals if a company wants, said Amy McDonough, who coordinates deals for Fitbit with companies. Other makers of wearable devices, including Jawbone, Samsung Electronics Co. (005930) and iHealth Lab Inc., have also targeted businesses.
Samsung leads the smart wearable-band market, according to a report today from Canalys. The researcher estimated the wearable band market grew almost eightfold in the first half of 2014 from a year ago.
Insurance Link
Some employers are encouraging the use of wearables without the gadgets being tied to lower insurance rates. Houston Methodist, owner of a chain of hospitals in the Houston area, got about 6,000 Fitbits this year and is offering employees the chance to win $10,000 if they walk more steps than the company’s top executives. Fitbit said it also works with Time Warner Inc. (TWX) and Autodesk Inc. (ADSK)
“Walking alone isn’t going to beat diabetes, but it’s certainly going to help,” said Marc Boom, chief executive officer of Houston Methodist. “Being more active results in better health. That’s indisputable.”
Scotty’s Brewhouse
At Scotty’s Brewhouse in Indianapolis, where the $15 “Big Ass Brewhouse Burger” includes four quarter-pound beef patties and American cheese, owner Scott Wise offers an extra day of vacation for managers at his 11 restaurants who use a Jawbone UP device to log an average of 10,000 steps a day for three months. That has some managers like Brian Winnie exercising more to earn time off for a trip he wants to take to Memphis, Tennessee.
“Outside of work, I picked up riding my bike to add extra steps that way,” Winnie said in an interview.
Despite some early enthusiasm, many companies are waiting to see whether the use of wearables is a fitness fad. No major research has been done that shows the use of these devices leads to lower health-care costs and many employers want to know “if this is something that’s a passing trend or something that has staying power and can have proven results,” said Eric Herbek, who runs digital engagement for Cigna.
The gadgets have been worthwhile for Chris Barbin, CEO of Appirio Inc. in San Francisco. He said about 40 percent of his staff, which numbers around 1,000, participates in a voluntary fitness program that includes uploading their activity with Fitbit.
$300,000 Discount
While health costs weren’t the priority for the program, Barbin said that by sharing the data with the company’s health care provider he negotiated $300,000 off his company’s roughly $5 million in annual insurance costs by showing his staff is getting healthier. He said privacy protections are in place for those who want to keep the data secret. The program has become one of the most popular forums on Appirio’s internal social network, he said.
“We had an initial batch of data about people who had lost weight, and people who had moved from high risk to moderate risk,” he said. “When we could show all that information to our insurer, that’s pretty powerful.”
Kristi Slagle, whose husband slimmed down through BP’s program, isn’t concerned about privacy with the gadgets. She said the program injects more fairness into the system because those who are healthier currently end up shouldering more costs for those who aren’t.
“I like that BP is making people more accountable,” she said.
To contact the reporter on this story: Adam Satariano in San Francisco atasatariano1@bloomberg.net

Natural Tricks to Falling Asleep
Natural Tricks to Falling Asleep
From our wellness partner, Cleveland Clinic
 Try These Natural Tricks to Fall Asleep More Easily
Try These Natural Tricks to Fall Asleep More Easily
Seeing a physician for help with your sleeping problems? You might want to try complementary medicine as another way to help you get back to restful slumber.
Complementary medicine refers to forms of non-invasive therapies that a patient can use alongside conventional Western medicine. Nearly 40 percent of Americans use this approach for specific conditions or overall well-being, says the National Institutes of Health (NIH).
“Many complementary therapies have been shown, through high-quality scientific evidence, to be safe and effective,” says integrative medicine specialist Melissa C. Young, MD. She sees patients at Cleveland Clinic’s Center for Integrative Medicine.
Complementary therapies for insomnia comprise four categories: mind-body therapies, body-based therapies, biologically based therapies and cognitive-behavioral therapy.
Here’s a rundown of the four categories and how you can leverage them to get back to sleep:
Mind-body therapies
The mind is a key player when it comes to how easily you fall asleep and stay asleep. This is why people should try mind-body techniques first when they experience insomnia, Dr. Young says.
Examples of mind-body techniques include meditation, hypnosis, guided imagery, tai chi and yoga. These practices can help to calm people’s thoughts and help them to relax. They are particularly helpful for older adults.
Body-based therapies
Body-based therapies can relax the body enough so that it is ready for sleep. These include massage and acupuncture, as well as energy techniques for stress reduction. Massage benefits everyone from infants to older adults and cancer patients. Acupuncture enhances sleep quality, especially if you’re feeling pain. Energy techniques include reiki, healing touch and therapeutic touch.
Biologically based therapies
Biological supplements aren’t sleeping pills. They help to balance your body’s chemistry and rhythm naturally, and make it easier to fall asleep.
Dr. Young says the most effective and popular biological treatments are:
- Magnesium, a mineral supplement
- Melatonin, a hormone that plays a role in sleep
- Chamomile tea
- I-theanine, a naturally occurring amino acid
Cognitive-behavioral therapy
Cognitive behavioral therapy for insomnia is a group of strategies that can help you to fall asleep faster, stay asleep and improve your sleep quality. At the same time, these strategies increase the overall amount of time you sleep. Cognitive-behavioral therapy is effective in the short- and long-term, and has minimal side effects.
“It helps people change the thoughts and behaviors that interfere with sleep,” says Michelle Drerup, PsyD, of the Cleveland Clinic Sleep Disorders Center.
Dr. Drerup gives these suggestions:
- Limit the time you spend awake in bed. If you find yourself still awake after 15 to 20 minutes, leave the bedroom and return when you feel tired. You should associate your bedroom only with sleep — not TV, emails from work or worry.
- Create a sleep schedule—and stick to it. Wake up at the same time each day, no matter your nightly experience. This will help your body regulate its internal 24-hour sleep-wake cycle, otherwise known as your biological clock or circadian rhythm.
- Practice good sleep hygiene. Part of getting good sleep is having healthy habits. Get regular exercise (but not too close to bedtime), develop a pre-bedtime relaxation routine, avoid or limit caffeine, avoid or limit naps to 30 minutes and limit your intake of alcohol.
- Study up on sleep. It’s easier to change sleep habits when you know how and why people sleep, and which beliefs, behaviors and outside influences affect your sleep.
- Consider cognitive therapy. Five mental processes influence insomnia: worry, selective attention and monitoring, distorted perception of sleep and daytime deficits, unhelpful beliefs about sleep and counterproductive safety behaviors. Cognitive therapy helps you to reverse these mental processes. Cognitive therapy is especially helpful in preventing relapse.
- Relax. This is often easier said than done. This is why relaxation training from a sleep psychologist or a professional trained in services such as meditation, guided imagery or hypnosis may help. Results are not immediate, but last a lifetime.
More information
Licensed Brokers vs Navigators
Licensed Brokers vs Navigators
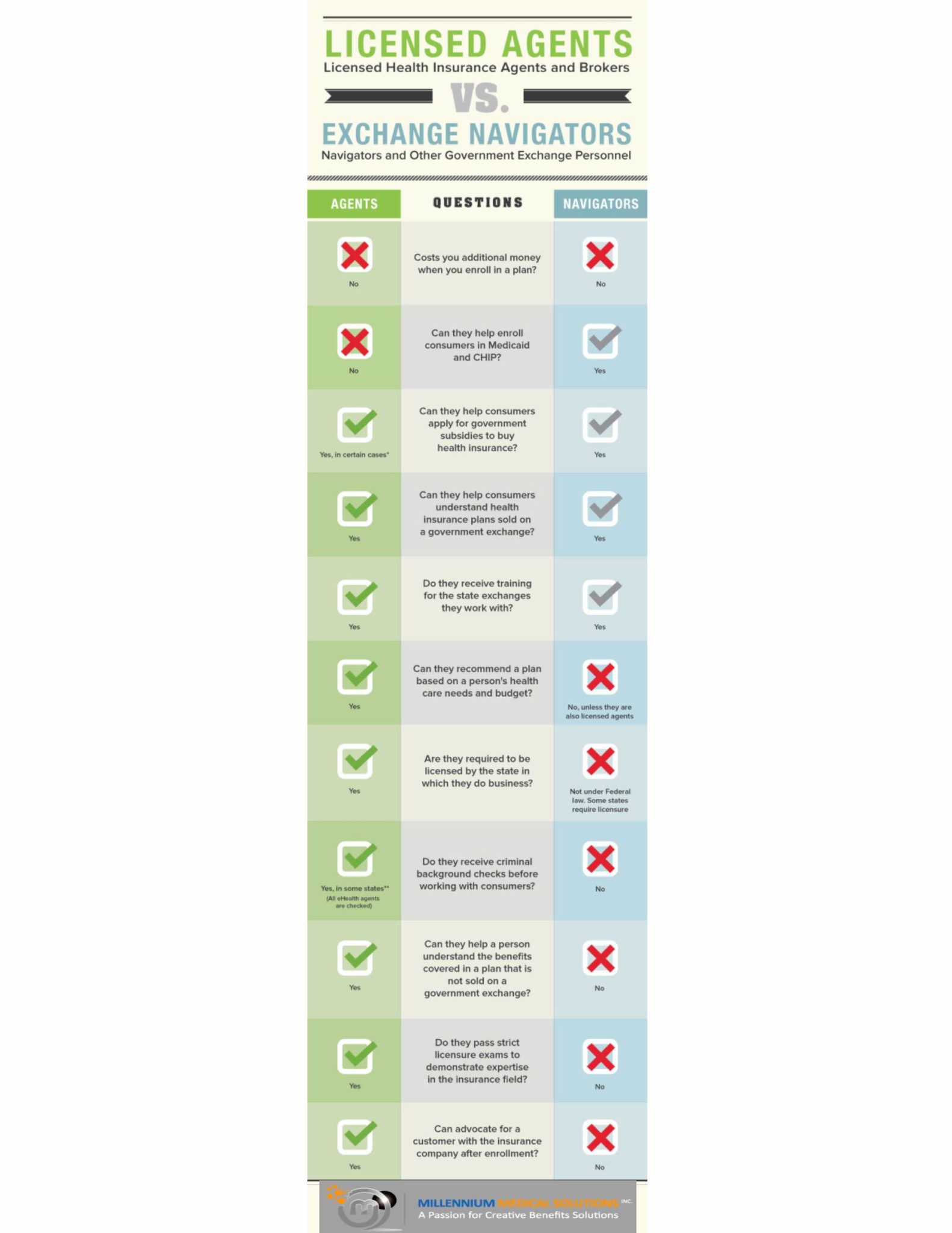
With less than 45 days before the first Affordable Care Act Open Enrollment set to end its important to understand the role of both Brokers and Navigators. The Patient Protection and Affordable Care Act (PPACA) requires States to establish a “Navigator” Program to help educate consumers about Health Exchange marketplace. With the new health insurance exchanges a broker can act either as a traditional broker or a navigator (but not both). The info-graph below illustrates how navigators will differ from brokers.
 Specifically, agents and brokers play a vital role in the developing health insurance exchanges nation wide. As the individuals with the education and expertise to advise and help select health insurance products for families and businesses large and small, health insurance agents, brokers and consultants occupy a unique place in the health care coverage system.
Specifically, agents and brokers play a vital role in the developing health insurance exchanges nation wide. As the individuals with the education and expertise to advise and help select health insurance products for families and businesses large and small, health insurance agents, brokers and consultants occupy a unique place in the health care coverage system.
We educate consumers on their health care coverage choices, help them select the most appropriate plans for their specific needs, and serve as their advocate if problems should arise. Subject to strict state licensing laws and education requirements, agents, brokers and consultants are critical to not only the health insurance enrollment process, but also in serving the healthinsurance coverage needs of individuals and employers after the point of sale.
Benefit specialists design benefit plans, explain coordination issues of public and private benefits to individuals and employees, and solve complex claims and billing issues. We help design and implement cutting-edge health promotion and wellness programs and help our clients comply with state and federal laws like newly enacted PPACA, HIPAA, COBRA and ERISA.
Professional agents, brokers and consultants continue to assist individuals and small businesses with their coverage needs long after the point of sale. Whereas a travel agent is finished with a client after the travel is completed, benefit specialists continues to serve as compliance experts, health and wellness promoters and the prominent contact for complex claims and billing issues. Health insurance coverage is a longstanding commitment for American consumers and often requires guidance from benefit specialists when dealing with a complex healthcare system.
For more information regarding both Exchanges – Individual Exchanges or SHOP please contact our team at Millennium Medical Solutions Corp (855)667-4621. We work in coordination with Navigators to assist with medicaid, CHIP Child Health Plus, Family Health Plus and Medicare Dual Eligibles. We have Spanish, Russian, and Hebrew speakers available. Quotes can also be viewed on our site.See Health Reform Resource
2014 A New Year in Health Care Reform
[fusion_text]
2014 – A New Year in Health Care Reform
After three (3) years of spirited debate, numerous lawsuits, and a Supreme Court ruling, the individual mandate kicked in January 1, 2014. Individuals must have health insurance or pay a tax (as defined by the Supreme Court). As an employer what should you be prepared for this year?
It has been an eventful year for the American health care system, to say the least. More parts of the Patient Protection and Affordable Care Act (PPACA) have gone into effect and the launch of the health care exchanges across the country is now under way. There have been numerous challenges to the PPACA and many of its components. The U.S. Supreme Court has ruled the Act’s individual mandate constitutional, but continues to examine the constitutionality of other aspects of the law.
Insurers have shifted more and more of the health care cost burden to enrollees through high deductible, higher co-pays and fixed benefits plans. An increasing number of payers are using Medicare based pricing, data analytics and wellness programs in their efforts to control ever rising costs. Narrow networks are popping up across the country as a vehicle for cost control.
Whatever the New Year brings, we look forward to supporting you in your continuing efforts to control costs while maintaining a high standard of care.
The New Year Ushers in Health Care Reform
- All employers will have to pay additional taxes on their health insurance plans which may result in about a 5% average increase in premiums.
- Waiting periods for benefits may not exceed 90 days from the date of hire. This will be effective with your 2014 renewal.
- Small group employers (2-50 employees) will have to include pediatric dental and vision in their 2014 health plans.
- Small employers who qualify for the Small Business Health Care Tax Credit, and want to take advantage of the tax credit, must purchase their health insurance through the SHOP Marketplace. Yes, as your broker, we can assist you with the SHOP Marketplace.
- Applicable Large Employers are employers with 50 FTE (full-time equivalents) or more, and must offer affordable and minimum value coverage to full-time employees (employees who work 30 hours or more per week). Employers must offer minimum value coverage to dependents, but do not have to meet the affordable test. Employers are not required to offer coverage to spouses. Penalties for not offering coverage have been delayed until 2015. However, we do not know if penalties will begin January 1, 2015 or with the 2015 health insurance renewal; awaiting a response from the IRS.
- Applicable Large Employers who have variable hour employees, employees who have a fluctuating schedule, should select a measurement period (3, 6, 9, 12 months) and begin tracking hours to determine if variable hour employees meet the 30 hour requirement.
- Employers who issued 250+ W-2 forms for the 2012 tax year will need to include the cost of health insurance on their W-2 forms for the 2013 tax year. Other employers may voluntarily include the cost of health insurance on their employees’ W-2 forms.
Individuals who do not have coverage in 2014 will be subject to a penalty which will be calculated one of two ways, whichever one is higher applies.
- $95 per person, $47.50 for individuals under 18; the maximum penalty for a family under this calculation is $285.
- 1% of yearly household income; the maximum penalty is the national average yearly premium for a bronze plan.
- The fee increases every year. In 2015 it’s 2% of income or $325 per person. In 2016 and later years it’s 2.5% of income or $695 per person. After that it is adjusted for inflation.
Individuals who are uninsured for just part of the year, 1/12 of the yearly penalty applies to each month the individual is uninsured. Individuals who have coverage for one (1) day during a month will be considered to have coverage and not pay a penalty for the month. Individuals who have a short gap in coverage, who are uninsured for less than 3 months, may not be required to pay a penalty for those months.
Health Care Reform 2014 Compliance Checklist – Click Here.Please contact us if you have questions, if you need assistance with SHOP Marketplace, or you have employees who need assistance getting individual coverage to avoid the penalty.
[/fusion_text]


