by admin | Jun 25, 2012 | Health Care Reform, Obamacare, PPACA
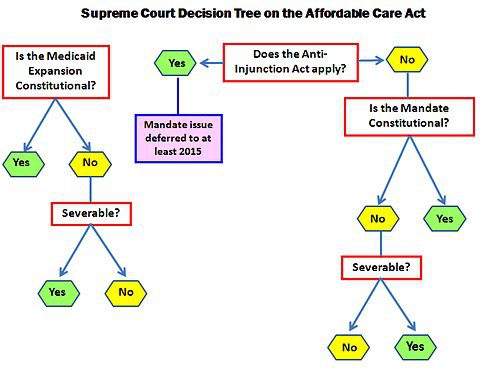
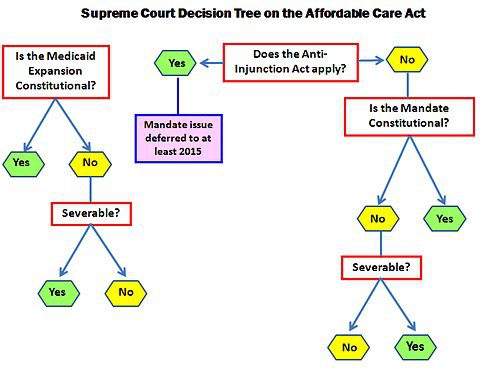
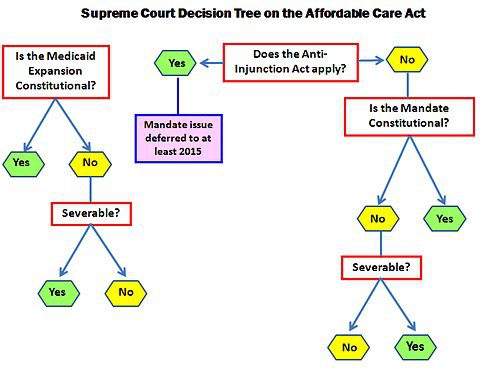
The biggest Supreme Court Ruling in a decae is expected this Thursday before the Summer recess. Yet thats when the fun begins.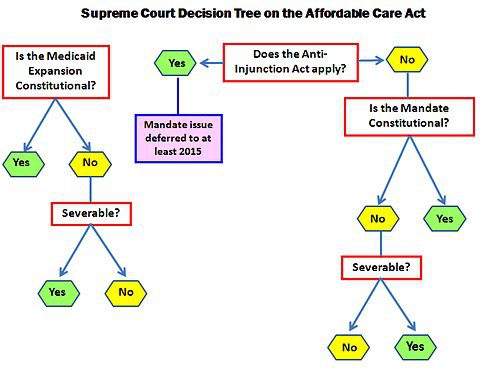 Possible outcomes: Possible outcomes:- Delay hearing the legal issues associated with case for several years due to the Tax Issue.
- Invalidate the Individual Mandate.
- Invalidate all or part of the Medicaid Expansion requirements.
- Uphold PPACA as is.
- Declare the entire Act unconstitutional due to the lack of a Severability Clause if any of the key provisions such as the Individual Mandate overturned.
If individual mandate is repealed but leave other PPACA provisions in place, this outcome could greatly limit the coverage goals underpinning the Affordable Care Act and cause significant problems in the health insurance markets. For example, MIT economist Jonathan Gruber said, “Without a mandate the law is a lot less effective. The market will not collapse, but it will be a ton more expensive and cover many fewer people.” While States such as NY may follow Massachusetts and set up their own Individual Mandate this becomes challenging with less Federal funding. Funding for the individual market place subsidy with subsidies could collapse. See subsidy calculator here. Eliminating the mandate would increase premiums and mean that far fewer of the uninsured would be covered. This is known as adverse selection where the sick population would be willing to pay higher premiums and forcing the healthy population to opt out of exchange. States such as NY in fact have seen the Individual Market spiral out of control as they are high risk adverse group in order to supplement the preferred guaranteed non-preexisting condition group marketplace. Furthermore, NYS requires guaranteed issue for pre-existing condition for individual members with prior coverage.
If the court invalidates the individual mandate and leave rest of Act in tact it may lead to a death spiral. Popular reforms such as overage 26 dependent coverage and expected pre-existing condition waiver in 2014 would possibly be dismantled. The decision would punt health-care reform back to Congress, which “isn’t doing anything this year” and thus create major uncertainty going into the November elections. Taxes on pharma and medical devices would remain, while managed-care and hospital companies would suffer big losses. Insurers would be forced to take on sick patients without benefitting from the healthy ones who would have been enrolled under the mandate. In this scenario, a lot of companies would simply cut their losses and leave the individual insurance market altogether; the law would essentially “run them out of business. Either way the lack of uncertainty has delayed hospitals and insurers from new hires and taking decisive actions. Same time next week we hope to celebrate July 4th with certainty. |

by admin | Jun 12, 2012 | Health Care Reform, Hospitals, PPACA

Accountable Care Organization
NYU Beth Israel Hospital Merger and ACO
Accountable Care Organization
As reported in NYT last week – New York Hospitals Look to Combine, Forming a Giant “The proposed merger would bring together NYU Langone Medical Center, a highly specialized academic medical center, and Continuum Health Partners, a network of several community-oriented hospitals, including Beth Israel and the two St. Luke’s-Roosevelt campuses.”
Anticipating changes in the way health care is paid for and delivered abound. WIth new Health Care Reform law the traditional fee-for-service model is being sacked in favor of patient care coordination. The consolidations by hospitals are needed in order to deliver the scales build on the ACO model of using independent providers/facilities.
Accountable Care Organization (ACO) – These organizations coordinate patient care and provide the full range of health care services for patients. The health reform law provides incentives for providers who join together to form such organizations and who agree to be accountable for the quality, cost, and overall care of Medicare beneficiaries who are enrolled in the traditional fee-for-service program who are assigned to the ACO.
The fee-for-service system has evidentially driven costs by incentivizing volumes of added procedures. The ACO model is built on par excellence hospitals such as Mayo Clinic where there is team of providers are financially incentivized for patient care coordination outcomes and high quality of care. The ACO’s payment would be tied to achieving goals that improve health care and save money. Members of the ACO would divvy up that payment. Today’s payment system, investments in providing better care are doubly penalized. If a hospital hires a nurse to follow up with patients after they are discharged in order to reduce readmissions — for example, to help patients with diabetes improve blood sugar control — it must pay for the nurse, which is typically not reimbursed by insurance companies or Medicare, and it loses revenue by preventing the readmission.
Congress included ACOs in the health care law as a way to rein in Medicare spending. That federal program pays for health care for people 65 and older and the disabled. The federal government estimates ACOs could save the Medicare program up to $940 million over four years. Medicare recently began testing this system with 32 pilot ACOs in 18 states, including one in the New York City area – Bronx Accountable Healthcare Network.
Some have pointed to ACO Model just as a pro-merger supporting argument with the FTC. These significant mergers create market dominance and therefore limit competition and drive up health care dollars. And yet Hospitals operate on thin profit margins and cannot afford to lose market share therein lies is the conundrum.
Addendum news: July 18, 2012 – Aetna and Hunterdon HealthCare Partners Forge New Accountable Care Relationship
by admin | Mar 12, 2012 | Health Care Reform, healthcare, Hospitals, PPACA, Small Business Group Health

Out of Control Out of Network Charges
Few healthcare changes have been more impacted than the out of control out of network charges billed to patients. The health care reform bill known as PPACA has for the most part been insignificant in the Northeast, in particular, as many state laws have already addressed issues such as pre-existing conditions, contraception, coverage rescissions and maximum loss ratios (MLR).
Instead, the market forces are reshaping the medical field into significant insurance & provider consolidation, larger hospital groups and flattening provider reimbursements. The problem is pointed out in Out of Network Medical Costs Affecting NY State Across investigation report commissioned by Governor Cuomo recognizing the unexpected out-of-network claim problem. Officials say that this is now “an overwhelming amount of consumer complaints.” Some examples cited in the report An Unwelcome Surprise – “a neurosurgeon charged $159,000 for an emergency procedure for which Medicare would have paid only $8,493.” Another example: ” a consumer went to an in-network hospital for gallbladder surgery with a participating surgeon. The consumer was not informed that a non-participating anesthesiologist would be used, and was stuck with a $1,800 bill. Providers are not currently required to disclose before they provide services whether they are in-network.” The average out-of-network radiology bill was 33 times what Medicare pays, officials say.
To make matters worse, Health Insurers have reduced their out of network recognized charges from private industry index UCR (usual customary and reasonable) to the Medicare Index known as RBRVS ( Resource Based Relative Value Scale ). Insurers moved away from UCR after then-NYS D.A. Mario Cuomo in 2009 forced Unitedhelatcare Group (owners of Inginex) to settle $50 Million in a conflict of interest allegation. D.A. Cuomo future hopes for UCR were to that it be overseen by a non-profit entity. So much for best laid plans.
Today, 90% of SMB members have in network only benefits but the few remaining consumers are paying for eroding out of network benefits with little transparencies and necessary protection from new out of network billing practices. The NY Dept of Financial services is calling for providers in non-emergency situations to disclose whether or not all services are in-network, what out-of-network charges will be and how much insurers will cover.
Insurers such as Aetna are taking action – with lawsuits throughout the country such as Aetna sues 9 N.J. doctors for “unconscionable” fees. Another Aetna lawsuit is discussed extensively in a law blog: In New Lawsuit, Health Insurers Allege Fraud and Kickbacks Against Out-of-Network Providers Who Forgive Patients’ Financial Responsibility.
In an ominous statement” “Failure to recognize this historical out-of-network avalanche will result in shocking financial disasters, as experienced by so many hospitals in 2003″
by admin | Jan 8, 2012 | Health Care Reform, healthcare, NY News, Small Business Group Health, State Exchanges
In the wake of Empire Blue Cross’s recent major SMB changes the 2 new Crains article below point to the early shake up results.
Tough Decisions on Health Coverage
Insurance Good Luck
Empire’s Small Group “simplification” did indeed cause groups to escape Empire’s rate increases and reduced plan selections. Additional, not mentioned in the article was that groups are facing plan modifications such as Rx changes switch to % from fixed $ copay and loss of Walgreen/Duane Reades chains. By being the largest insurer on the block heavy provider negotiations have been de rigieur as evidenced by loss of Westchester Medical Center for 14 months and counting.
Groups have been fortunate to find comparable alternatives despite these changes but we see little public evidence of concern form NYS legislature. We are not seeing the long term vision to open up markets to strong national insurance competitors. On the contrary we have deep concerns of allowing the past 2 non-profits of GHI and HIP merger and latest talks of going for profit.
Lastly, the article makes mention of possible “Health Exchanges” entering the market and lowering rates. Where is there evidence of this decrease? I’m not seeing why an insurer working in an oligopoly environment with price controls would be motivated to lower rates. Would Con Ed or Blue Bell lower rates in the 70s because now SMB can shop online??
![CLASS In or Out? – Long Term Care]()
by admin | Sep 23, 2011 | PPACA

In another downsizing move of the Health Care Reform ACT – Patient Protection and Affordable Care Act (PPACA) the office responsible for the new Long Term Care Act claus have been reassigned. This portion of the law is known as CLASS (Community Living Assistance Services and Supports) that was intended to make private Long Term Care Ins more affordable and available through the work site.
There are Long Term Care concerns as less than 10% of the US Consumers carry a LTC policy. Part of the disparity is obvious costs and part is the feeling that Public Gov will take care of this. In order for Medicaid to pay for Nursing Homes though ones assets with some exceptions are liquidated. The other is not realizing that LTC does cover Home Health Care.
Under the CLASS provision “the Secretary shall designate a benefit plan no later than October 1, 2012.” However, with this week’s action of “reassigning” 8 members of the CLASS unit go is another step in diminishing the act. Also, politically before an election year it would of given too much fodder for the Republican Party. To have CLASS succeed, HHS would have to make it affordable, but, because the CLASS Act plan would be a voluntary plan, the plan would could face enormous risk of adverse selection, with only unhealthy workers signing up. Critics contend that the program managers would have to raise premiums substantially over time to keep the program solvent, and that, over time, the program would fall into a costly deathly spiral. The program has become a favorite target for Republicans.
There may be political winners and losers but sadly who can calculate the amount of time + resources wasted to land back to square 1?
Resources:
http://www.washingtontimes.com/news/2011/sep/22/obama-pulls-back-part-affordable-care-act/
http://blogs.wsj.com/washwire/2011/09/22/long-term-care-program-in-jeopardy/?mod=WSJBlog

by admin | Sep 1, 2011 | group health insurance, Health Care Reform, healthcare, PPACA, Small Business Group Health
UnitedHealthcare Buying Medical Groups?

Optum Health owned by UnitedHealth Group
Today’s WSJ reports UnitedHealth Buys California Group of 2,300 Doctors may be a signal of future trends in healthcare where there is blurring of the lines between insurers and providers. The article goes on to to mention that United Healthcare has stated that providers acquired by Optum will not work exclusively with United’s health plan, and will continue to contract with an array of insurers.
The article goes on to state that “the potential complications that might ensue, Monarch is currently in an arrangement with United competitor WellPoint Inc. to create a cooperative “accountable-care organization” aimed at bringing down health-care costs and improving quality.”
In the aftermath of Health Care Reform, insurers profits will be curtailed. New price limitations imposed by MLR (Maximum Loss ratios) where 85% of large group premiums collected must be spent on healthcare services(claims) and health quality improvement . New state tax surcharges such as New York’s 82% of above MLR applies to small groups. In fact in NY the cost of doing business is a staggering 16%+ added to the usual corporate tax. See The NYS Surcharge.
Additionally, the industry as a whole will be paying an annual tax to help pay for PPACA(Patient Protection Affordability Care Act). This tax rises from $8 billion in 2014 to $14.3 billion in 2018 and in later years, even higher according to a complex index. See Kaiser Bill Summary .
While its unglamorous to defend insurers they are clearly paying their share and like it or not they are good at health care management. Unlike foreign HQ tax loop holes taken advantage by companies such as G.E. , an insurer cannot place patent rights in Zug, Switzerland and take advantage. Each of these taxes is increased regularly by the State and contributes significantly to annual increases in rates. The competition in the health insurance industry is already at a dangerous low levels. Negotiating with insurers has become an overwhelming challenge in the large group market. Hospital groups have merged to mirror this Oligopoly trend and contractual issues are the new normal. See Empire & Stelllaris Reach pact.
So what to do other than to find profits elsewhere? Many issues and questions will abound as to the antitrust nature of this action. A similar issue appeared in the 90s Merck-Medco merger between a pharmaceutical and mail order PBM. The conflict of interest claims will abound, how do you negotiate one provider group owned by United-Healthcare as opposed to one owned by HealthNet? Will insurer share competitive insights with other practices? Are small independent Dr. Groups completely left out of the loop and feel pressured to be bought out? Will the insurers medical group have unfair advantage in buying out the smaller physician practice? Perhaps in the same vein of the Merck-Medco analogy the health insurer shareholders will do well for a decade and then simply split up?
Its all too early to tell but this much is clear, there aint no money in running a health insurance management company today.
 Possible outcomes:
Possible outcomes: