Update: Oxford/United and Mt Sinai Health Systems Split
Recently, UHC/Oxford and Mt Sinai Health System had split effective January 1, 2024. Since that time there have been a state-required cooling-off period and ongoing talks on resolution but that has not yielded a positive outcome yet. The Mount Sinai Hospital, Mount Sinai Queens, and their related hospital outpatient locations will remain in-network for all patients until at least Friday, March 1.
According to UnitedHealthcare/Oxford:
- People enrolled in UnitedHealthcare fully insured commercial plans have continued network access to all of Mount Sinai’s hospitals through Feb. 29, 2024, due to New York cooling-off requirements.
- Unless they obtain admitting privileges to another in-network hospital, the majority of Mount Sinai’s physicians will no longer participate in our network for employer-sponsored and individual plans, including the Oxford Health Plan, effective March 22, 2024.
- This negotiation only impacts our relationship with Mount Sinai for employer-sponsored and individual commercial plans, including Oxford. All other active contracts, including Medicare Advantage and the Empire Plan, remain in place with no change.
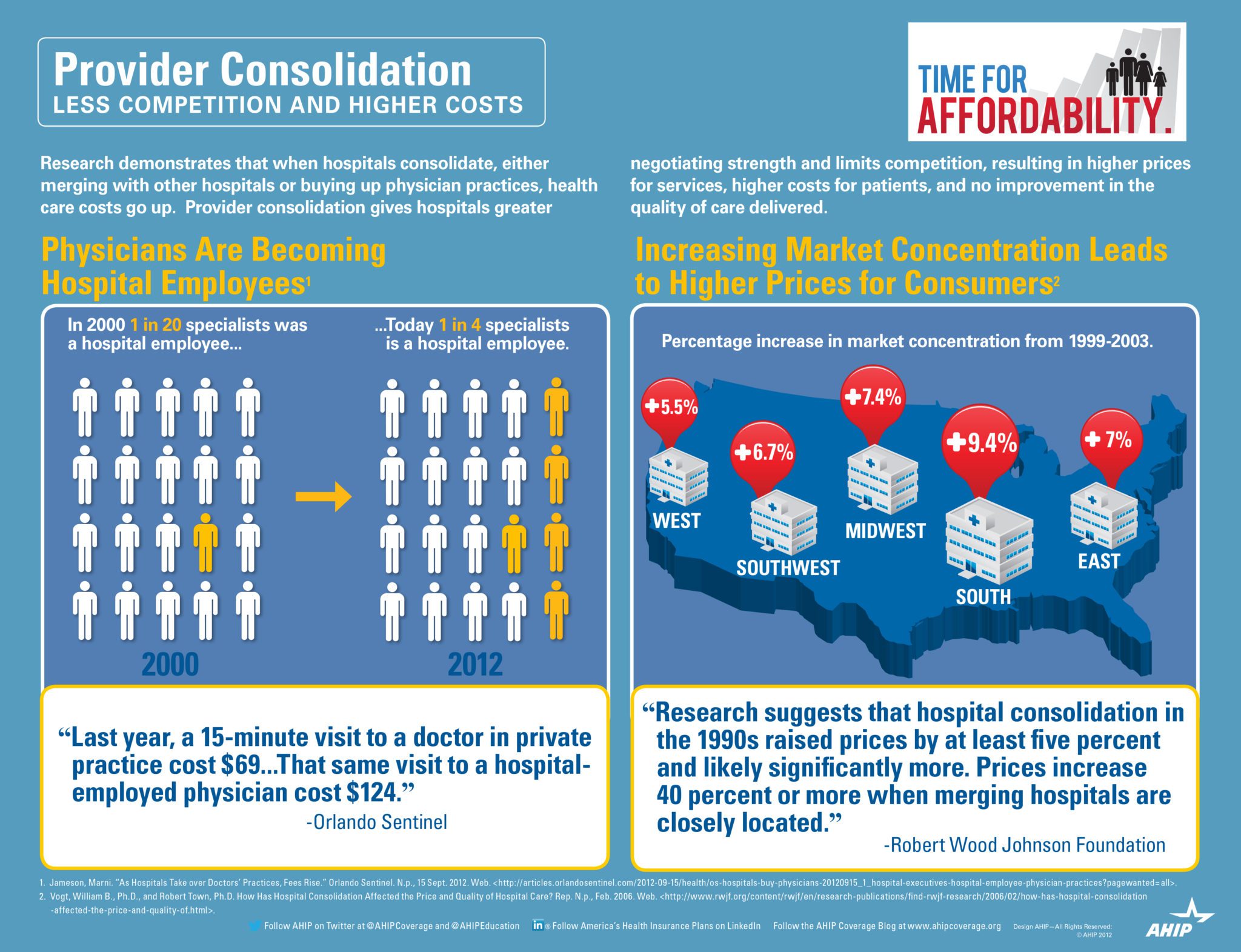
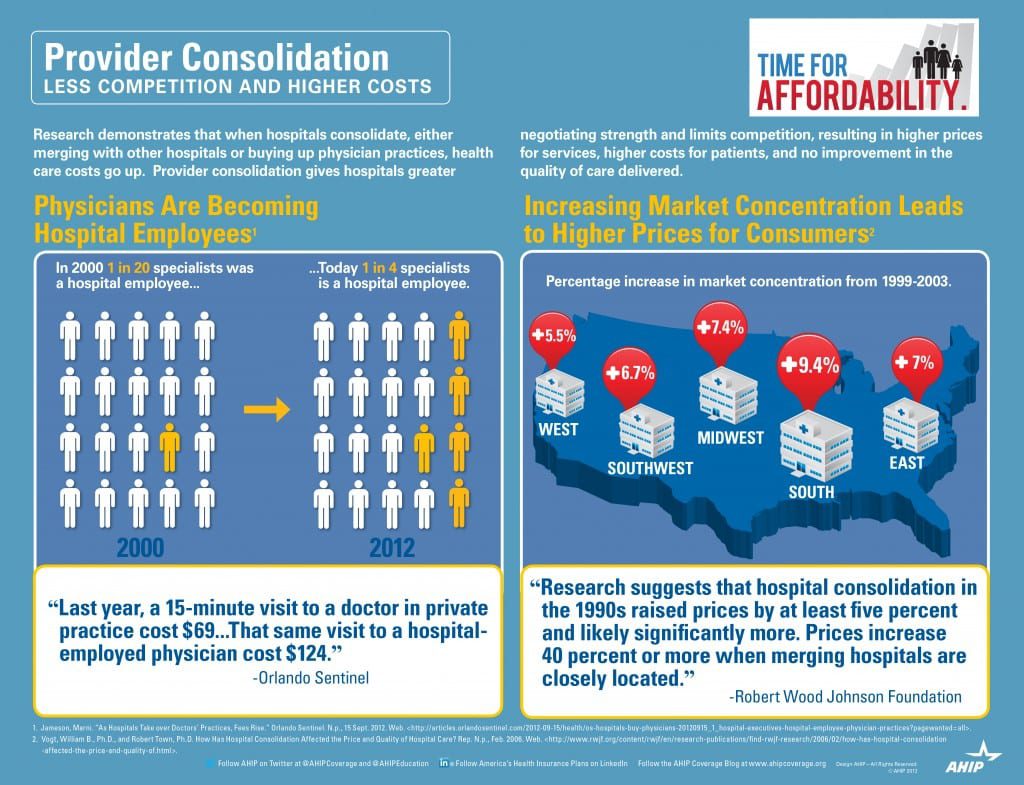
The two organizations had a three-year agreement that took effect on Jan. 1, 2022, which was canceled before it was supposed to expire amid a dispute over payment rates. Both institutions are blaming one another for the standoff.
Mount Sinai claims UnitedHealthcare compensates it an average of 30% less for care than other health systems in New York. The insurer pays New York-Presbyterian $25,911 for a normal vaginal birth, and Mount Sinai $15,989, Mount Sinai said.
“Mount Sinai must be paid fairly,” spokeswoman Lucia Lee said in a statement. “As Mount Sinai costs substantially less than our peers, UHC/Oxford will actually end up paying more for patients to get care at other systems in New York. This cost — estimated to be at least $140 million more over the course of a year — will be passed on to employers and patients.”
UnitedHealthcare says Mount Sinai sought “outlandish price hikes” that would increase costs for services an average of 50% over three years or $600 million — an estimate disputed by Mount Sinai. For example, a regular, outpatient colonoscopy at South Nassau costs about $6,000 and would be about $8,700 in three years under Mount Sinai’s proposal, according to UnitedHealthcare.
Mt Sinai Hospitals & Health System
| Facility Name | County |
| Mount Sinai Beth Israel | NYC |
| The Mount Sinai Hospital | NYC |
| Mount Sinai Morningside | NYC |
| The Mount Sinai West | NYC |
| Mount Sinai-Union Square | NYC |
| Mount Sinai Kravis Children’s Hospital | NYC |
| Mount Sinai-Behavioral Health Center (MSBHC) | NYC |
| Blavatnik Center, Medical Center | NYC |
| New York Eye and Ear Infirmary of Mount Sinai | NYC |
| Mount Sinai Brooklyn | Brooklyn |
| Mount Sinai Queens | Queens |
| Mount Sinai South Nassau | Long Island |
Neighboring Hospitals
Bellevue Hospital Center | NYC | New York Presbyterian Queens | Queens |
Elmhurst Hospital Center | Queens | New York Presbyterian Weill Cornell | NYC |
Flushing Hospital Medical Center | Queens | North Shore University Hospital Manhasset | Long Island |
Lenox Hill Hospital | NYC | NYU Langone Hospital Brooklyn | Brooklyn |
Long Island Jewish Medical Center | Brooklyn | NYU Langone Hospital Long Island | Long Island |
Maimonides Medical Center | Brooklyn | St. Francis Hospital | Long Island |
Mercy Medical Center | Long Island | St. Johns Episcopal Hospital | Queens |
New York Presbyterian Columbia | NYC | St. Joseph Hospital | Queens |
New York Presbyterian Lower Manhattan Hospital | NYC | Wyckoff Heights Medical Center | Brooklyn |
Both sides need each other as both are market leaders in their fields. It is our hope and most of our clients that they get this resolved soon. In the meantime, please bookmark our site for the latest updates. And do reach out to us and learn the steps that you can take to smoothen this temporary roadblock.
Resources:
For information about transparency providers and new tech tools contact us at info@360peo.com or (855)667-4621.
Put You & Your Employees in Good Hands
Get In Touch
For more information on PEOs or a customized quote please submit your contact. We will be in touch ASAP.