by Alex | Aug 3, 2015 | group health insurance, Healthy NY, NY News, Small Business Group Health
NYS 2016 Rates Approved
The rate requests for 2016 marked the first year in which insurers could rely on actual data from exchange enrollees. In many cases, insurers participating in exchanges in other states requested double-digit rate increases. New York is the second-largest state to receive final approval of its rate requests. Earlier this week, California insurance regulators approving an average rate increase of just 4 percent.
To the relief of customers of industry leader Oxford/UnitedHealthcare the rate increase for groups will be 3.9 to 6.5%. Importantly, the rates are a collective average and may range depending on one’s particular health plan. Additionally, Helath Insurers can opt to tweak or remove plans. Reminder: be sure to check back again our site in 30-60 days. Rates will be posted upon Health Insurer’s release. Also 2016 Individual Exchange Marketplace opens Nov 15th.
Individual Market
On average, insurers requested a 10.4 percent increase in health insurance rates for 2016 in the individual market. DFS reduced that average increase more than 30 percent to 7.1 percent – which is below the approximately 8 percent average increase in health care costs.
Starting on January 1, 2016, New York will add a new Basic Health Plan a.k.a ” Essential Health Plan” to the plans that can be purchased by lower income New Yorkers through NY State of Health. Households at or below 150 percent of the federal poverty level ($17,655 for a household of one; $36,375 for a household of four) will have no monthly premium for the Basic Health Plan. Those with slightly higher incomes at 200 percent of the federal poverty level ($23,540 for a household of one; $48,500 for a household of four) will have a low monthly premium of $20 for each adult.
The Basic Health Plan will provide the same covered services as other plans offered on the Marketplace. The Basic Health Plan has no annual deductible and lower copayments, making health care even more affordable for hundreds of thousands of New Yorkers. For example, a person who earns about $20,000 a year and uses moderate health care services including an inpatient hospital stay, prescription drugs and doctor’s visits, will pay about $730 a year for premiums and out-of-pocket costs under the Basic Health Plan in 2016 as compared to about $1,830 in 2015 if they were enrolled in a Qualified Health Plan.
Small Group Market
On average, insurers requested a 14.4 percent increase in health insurance rates for 2015 in the small group market. DFS reduced that average increase by 32 percent to 9.8 percent. A number of small businesses will also be eligible for tax credits that would lower those premium costs even further.
2016 Small Group Rate Actions – Overall Summary
Company | Requested | Approved | Reduction |
|---|
| Aetna Life | 23.87% | 21.47% | -2.40% |
| CDPHP HMO* | -19.84% | -19.84% | 0.00% |
| CDPHP UBI* | 16.56% | 16.56% | 0.00% |
| Emblem HIP* | 29.74% | 29.74% | 0.00% |
| Empire Assurance | 8.70% | 3.40% | -5.30% |
| Empire HMO | 9.21% | 4.37% | -4.84% |
| Excellus* | 13.90% | 10.00% | -3.90% |
| Health Republic* | 20.00% | 20.00% | 0.00% |
| HealthNow* | 8.06% | 0.66% | -7.40% |
| Independent IHA* | -15.60% | -15.60% | 0.00% |
| Independent IHBC | -6.19% | -6.19% | 0.00% |
| Managed Health | 5.60% | 3.94% | -1.66% |
| Metro Plus* | -0.81% | -0.81% | 0.00% |
| MVP Health Plan* | 7.28% | 6.36% | -0.92% |
| MVP Services* | 16.71% | 15.90% | -0.81% |
| North Shore LIJ* | 3.27% | 3.27% | 0.00% |
| Oxford OHI | 13.61% | 6.75% | -6.86% |
| Oxford OHP | 10.58% | 3.90% | -6.68% |
| United UHIC | 18.79% | 11.61% | -7.18% |
| All Companies Combined | 14.41% | 9.80% | -4.61% |
You may view the DFS press release, which includes a recap of the increases requested and approved by clicking here.
For specific details on all available health plans in 2015, contact our team at Millennium Medical Solutions Corp (855)667-4621. We work in coordination with Navigators to assist with Medicaid, CHIP Child Health Plus, Family Health Plus and Medicare Dual Eligibles. We have Spanish, Russian, and Hebrew speakers available. Quotes can also be viewed on our site.
See Health Reform Resource
NYS 2015 Rates Approved

by admin | Sep 7, 2014 | group health insurance, Health Care Reform, individual health insurance, NY News
NYS 2015 Rates Approved 
The NYS Department of Financial Services has reviewed individual and small group health carriers’ rate increase requests for 2015, and announced the results of their review.
Interestingly, North Shore LIJ Care Connect was the only insurer to request a rate reduction. With significant expansion steps they are well positioned for Wescthester, Bronx, NYC, SI, Queens and LI. These numbers are across the board and specific plan rate renewal may vary.
Reminder: Individual Exchange Marketplace opens Nov 2015. Rates will be posted upon Health Insurer’s release, check our site.
Individual Market
On average, insurers requested a 12.5 percent increase in health insurance rates for 2015 in the individual market. DFS reduced that average increase more than in half to 5.7 percent – which is below the approximately 8 percent average increase in health care costs.
Small Group Market
On average, insurers requested a 13.9 percent increase in health insurance rates for 2015 in the small group market. DFS reduced that average increase more than in half to 6.7 percent – which is also below the approximately 8 percent increase in health care costs.
You may view the DFS press release, which includes a recap of the increases requested and approved by clicking here.
For specific details on all available health plans in 2015, contact our team at Millennium Medical Solutions Corp (855)667-4621. We work in coordination with Navigators to assist with medicaid, CHIP Child Health Plus, Family Health Plus and Medicare Dual Eligibles. We have Spanish, Russian, and Hebrew speakers available. Quotes can also be viewed on our site.
See Health Reform Resource

by admin | Jul 28, 2014 | group health insurance, Health Care Reform
IRS Releases Draft of Employer Reporting Form for Health Reform Law Compliance
Business Insurance
Story by Matt Dunning

Click Above
July 28, 2014
The Internal Revenue Service has issued draft versions of the reporting forms most employers will begin using next year to show that their group health insurance plans comply with the health care reform law.
The long-awaited draft forms, posted late Thursday afternoon to the IRS’ website, are the first practical application of employers’ health care coverage and enrollment reporting obligations under the Patient Protection and Affordable Care Act since the regulations were finalized in March.
The forms are the primary mechanism through which the government intends to enforce the health care reform law’s minimum essential coverage and shared responsibility requirements for employers.
Beginning in 2015, employers with at least 100 full-time employees will be required to certify that benefits-eligible employees and their dependents have been offered minimum essential coverage and that their employees’ contributions to their premiums comply with cost-sharing limits established under the reform law. Smaller employers with 50-99 full-time employees are required to begin reporting in 2016.
Additionally, self-insured employers will be required to submit documentation to ensure compliance with minimum essential coverage requirements under the reform law’s individual coverage mandate.
“In accordance with the IRS’ normal process, these draft forms are being provided to help stakeholders, including employers, tax professionals and software providers, prepare for these new reporting provisions and to invite comments from them,” the IRS said in a statement released Thursday.
The IRS said it expects to publish draft instructions for completing the reporting forms by late August and that both the forms and the instructions would be finalized later this year.
Last year, the Obama administration announced it would postpone implementation of employers’ minimum essential coverage and shared responsibility obligations under the reform law for one year, largely due to widespread complaints about the complexity of the reporting requirements.
Though several months have passed since the administration issued a simplified set of information reporting rules, many employers have delayed preparations for meeting the requirements until the forms and instructions are available for review, said Richard Stover, a principal with Buck Consultants at Xerox in Secaucus, New Jersey.
“A lot of employers really haven’t been doing anything about reporting requirements, even with the final regulations in place, because they were waiting for these forms,” Mr. Stover said. “This is something they’ve been anxious to see.”
 CLICK HERE TO DOWNLOAD PDF – IRS Releases Compliance Drafts July_2014
CLICK HERE TO DOWNLOAD PDF – IRS Releases Compliance Drafts July_2014
For more information contact us (855) 667-4621.
by admin | Aug 30, 2012 | group health insurance, Health Care Reform, PPACA
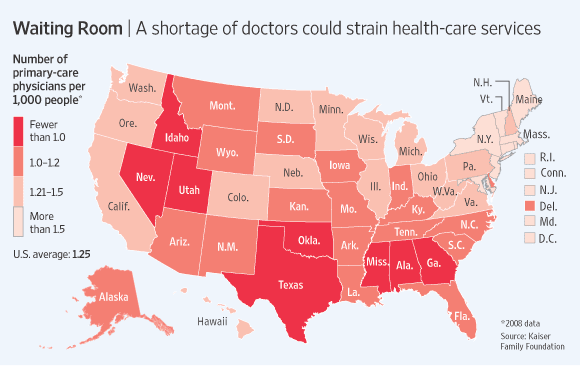
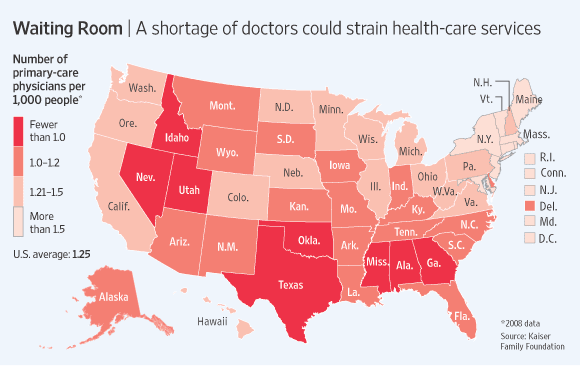
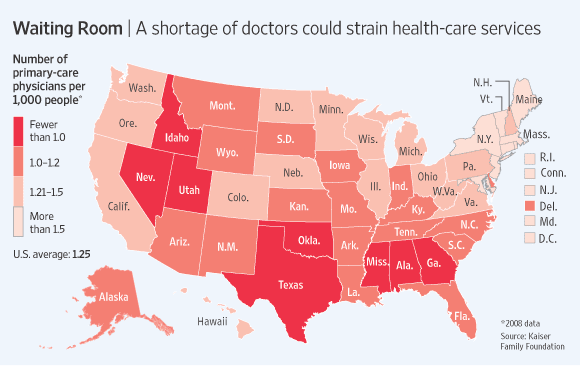
With increase in demand and already shortages of Doctors the Obamacare – Affordable Care Act will put significant severe strains on patient access.
According to todays WSJ article – John C. Goodman: Why the Doctor Can’t See You “Here is the problem: The health-care system can’t possibly deliver on the huge increase in demand for primary-care services. The original ObamaCare bill actually had a line item for increased doctor training. But this provision was zeroed out before passage, probably to keep down the cost of health reform. The result will be gridlock.”
The Department of Health and Human Services, estimated the minimum number of primary care physicians to ensure “adequate supply” at 60 to 80 per 100,000 population. By 2020 an estimated 45,000 new PCP would ne needed 2020. But the number of medical-school students entering family medicine fell more than a quarter between 2002 and 2007.
The greatest demand will be for primary-care physicians. These general practitioners, internists, family physicians and pediatricians will have a larger role under the new law, coordinating care for each patient.
“Take preventive care. ObamaCare says that health insurance must cover the tests and procedures recommended by the U.S. Preventive Services Task Force. What would that involve? In the American Journal of Public Health (2003), scholars at Duke University calculated that arranging for and counseling patients about all those screenings would require 1,773 hours of the average primary-care physician’s time each year, or 7.4 hours per working day.”
In 2014 an expected 30 Million people will be added The expected wait time would increase form 3 weeks to about 2 months. The 2 month estimate is a approximately how long it takes to schedule a check up in Boston which had enacted universal healthcare 5 years ago. Furthermore, the positive measures to encourage preventive care such as healthy screenings and well-care will only add to the gridlock.
“When people cannot find a primary-care physician who will see them in a reasonable length of time, all too often they go to hospital emergency rooms. Yet a 2007 study of California in the Annals of Emergency Medicine showed that up to 20% of the patients who entered an emergency room left without ever seeing a doctor, because they got tired of waiting.” Be prepared for that situation to get worse even with Urgent Care Centers.
“A New York Times survey of dermatologists in 2008 for example, found an extensive two-tiered system. For patients in need of services covered by Medicare, the typical wait to see a doctor was two or three weeks, and the appointments were made by answering machine.However, for Botox and other treatments not covered by Medicare (and for which patients pay the market price out of pocket), appointments to see those same doctors were often available on the same day, and they were made by live receptionists.”
As with any economic model the shorter supply of provider will drive up costs. Aside form provider fees increasing, those who can afford concierge service and pay $2,000-$4,000 may be able to get same day services and easy access but for most Americans with insurance will be waiting longer to see their Doctors. The irony is that people with coverage will have limited access to care.

by admin | Sep 1, 2011 | group health insurance, Health Care Reform, healthcare, PPACA, Small Business Group Health
UnitedHealthcare Buying Medical Groups?

Optum Health owned by UnitedHealth Group
Today’s WSJ reports UnitedHealth Buys California Group of 2,300 Doctors may be a signal of future trends in healthcare where there is blurring of the lines between insurers and providers. The article goes on to to mention that United Healthcare has stated that providers acquired by Optum will not work exclusively with United’s health plan, and will continue to contract with an array of insurers.
The article goes on to state that “the potential complications that might ensue, Monarch is currently in an arrangement with United competitor WellPoint Inc. to create a cooperative “accountable-care organization” aimed at bringing down health-care costs and improving quality.”
In the aftermath of Health Care Reform, insurers profits will be curtailed. New price limitations imposed by MLR (Maximum Loss ratios) where 85% of large group premiums collected must be spent on healthcare services(claims) and health quality improvement . New state tax surcharges such as New York’s 82% of above MLR applies to small groups. In fact in NY the cost of doing business is a staggering 16%+ added to the usual corporate tax. See The NYS Surcharge.
Additionally, the industry as a whole will be paying an annual tax to help pay for PPACA(Patient Protection Affordability Care Act). This tax rises from $8 billion in 2014 to $14.3 billion in 2018 and in later years, even higher according to a complex index. See Kaiser Bill Summary .
While its unglamorous to defend insurers they are clearly paying their share and like it or not they are good at health care management. Unlike foreign HQ tax loop holes taken advantage by companies such as G.E. , an insurer cannot place patent rights in Zug, Switzerland and take advantage. Each of these taxes is increased regularly by the State and contributes significantly to annual increases in rates. The competition in the health insurance industry is already at a dangerous low levels. Negotiating with insurers has become an overwhelming challenge in the large group market. Hospital groups have merged to mirror this Oligopoly trend and contractual issues are the new normal. See Empire & Stelllaris Reach pact.
So what to do other than to find profits elsewhere? Many issues and questions will abound as to the antitrust nature of this action. A similar issue appeared in the 90s Merck-Medco merger between a pharmaceutical and mail order PBM. The conflict of interest claims will abound, how do you negotiate one provider group owned by United-Healthcare as opposed to one owned by HealthNet? Will insurer share competitive insights with other practices? Are small independent Dr. Groups completely left out of the loop and feel pressured to be bought out? Will the insurers medical group have unfair advantage in buying out the smaller physician practice? Perhaps in the same vein of the Merck-Medco analogy the health insurer shareholders will do well for a decade and then simply split up?
Its all too early to tell but this much is clear, there aint no money in running a health insurance management company today.
by admin | Aug 18, 2011 | group health insurance, healthcare, Hospitals
After balancing the budget and announcing $2.4 trillion in government spending cuts over ten years, politicians and media pundit are insisting that it is only the beginning of the attack on health care, pensions and other social programs.
So why is balancing the budget and cutting medicare so bad for the Privately Insured? After all, the Democrats have made sure the automatic cuts leave Medicare benefits untouched, and the Republicans have blocked any new taxes.
Everyone is content right? Or so it seems. But the truth is that cutting payments to Medicare providers will mean some Americans are going to pay more. It may not be called a tax, but if you’re covered by private health insurance, money will be coming out of your pocket nonetheless.
Here’s how cuts in Medicare affects the rest: If a hospital provides a service that costs $1,000,000, and the government elects to pay just $980,000, the $20,000 gap doesn’t disappear. The hospital has to cover it somehow. It will likely do so by shifting the costs to commercial insurers, which eventually means higher premiums. This cost shifting is nothing new-it’s been happening for years-but more cuts will just make it worse.
NY Hospitals in particular have felt Federal Funding cuts for teaching hospitals over the last decade. This has been a contributing factor to St. Vincents declaring bankruptcy last January. Many surviving hospitals however have the size to negotiate effectively with private insurers to make up that funding short fall.
So guess who makes up that difference? The fact remains, if you don’t deal with underlying costs, you’re not fixing the problem, you’re just covering it up.





 Doctor Shortages-covered but less access?
Doctor Shortages-covered but less access?